Minnesota Administrative Rules
CHAPTER 4732, IONIZING RADIATION
DEPARTMENT OF HEALTH
| Part | Title |
|---|---|
| 4732.0100 | PURPOSE AND SCOPE. |
| 4732.0110 | DEFINITIONS. |
| REGISTRATION REQUIREMENTS | |
| 4732.0200 | REGISTRATION REQUIREMENTS FOR RADIATION-PRODUCING EQUIPMENT AND OTHER ELECTRONIC DEVICES THAT PRODUCE RADIATION. |
| 4732.0210 | REGISTRATION FEES. |
| 4732.0220 | GENERAL REQUIREMENTS FOR ALL FACILITIES. |
| 4732.0250 | RECIPROCITY FOR OUT-OF-STATE RADIATION-PRODUCING EQUIPMENT. |
| 4732.0275 | REGISTRATION OF SERVICE PROVIDERS. |
| 4732.0280 | SERVICE PROVIDER'S RESPONSIBILITY. |
| GENERAL ADMINISTRATION | |
| 4732.0300 | EXEMPTIONS. |
| 4732.0305 | PROHIBITED USES. |
| 4732.0306 | UNAUTHORIZED USES. |
| 4732.0308 | VARIANCE IONIZING RADIATION RULES. |
| 4732.0310 | DATA PRIVACY. |
| 4732.0315 | DELIBERATE MISCONDUCT. |
| 4732.0320 | EMPLOYEE PROTECTION. |
| 4732.0330 | RECORDS. |
| 4732.0335 | INSPECTIONS AND TESTING. |
| 4732.0340 | VIOLATIONS AND ENFORCEMENT REQUIREMENTS. |
| SHIELDING REQUIREMENTS | |
| 4732.0355 | GENERAL REQUIREMENTS FOR SHIELDING AGAINST IONIZING RADIATION. |
| 4732.0360 | SHIELDING PLAN. |
| 4732.0365 | ADDITIONAL SHIELDING REQUIREMENTS FOR DENTAL FACILITIES. |
| 4732.0370 | ADDITIONAL SHIELDING REQUIREMENTS FOR INDUSTRIAL FACILITIES USING RADIATION-PRODUCING EQUIPMENT. |
| 4732.0380 | SHIELDING REQUIREMENTS FOR ACCELERATORS. |
| 4732.0385 | CAUTION SIGNS. |
| DOSE LEVELS | |
| 4732.0400 | DETERMINATION OF ACCUMULATED OCCUPATIONAL DOSE. |
| 4732.0410 | OCCUPATIONAL DOSE LIMITS FOR ADULTS. |
| 4732.0415 | DOSE EQUIVALENT TO AN EMBRYO OR FETUS. |
| 4732.0420 | EXPOSURE OF MINORS. |
| 4732.0425 | PLANNED SPECIAL EXPOSURES. |
| 4732.0430 | DOSE LIMITS FOR INDIVIDUAL MEMBERS OF THE PUBLIC. |
| 4732.0440 | INDIVIDUAL MONITORING. |
| RADIATION SAFETY REQUIREMENTS | |
| 4732.0500 | REGISTRANT'S SAFETY RESPONSIBILITIES. |
| 4732.0505 | RADIATION SAFETY OFFICER RESPONSIBILITIES. |
| 4732.0510 | PROCEDURES AND SAFETY INSTRUCTION FOR FACILITIES. |
| 4732.0520 | QUALITY ASSURANCE PROGRAM. |
| 4732.0530 | ALARA PROGRAM. |
| 4732.0535 | RETAKE OR REJECT ANALYSIS PROGRAM. |
| 4732.0540 | RADIATION PROGRAM AUDITS. |
| 4732.0545 | UTILIZATION LOG. |
| 4732.0550 | RADIOLOGICAL PRACTICE STANDARDS. |
| 4732.0555 | X-RAY FILM PROCESSING REQUIREMENTS. |
| 4732.0560 | ORDERING OF DIAGNOSTIC RADIOGRAPHIC OR THERAPEUTIC PROCEDURES. |
| 4732.0565 | HEALING ARTS SCREENING. |
| 4732.0570 | OPERATOR REQUIREMENTS. |
| 4732.0575 | EXAMINATION REQUIREMENTS. |
| 4732.0580 | REGISTRANT REQUIREMENTS FOR OPERATORS IN FACILITIES USING X-RAY EQUIPMENT. |
| 4732.0585 | EQUIVALENT EXAMINATIONS. |
| 4732.0590 | INDIVIDUALS OPERATING X-RAY EQUIPMENT DURING TRAINING. |
| REPORTS AND NOTIFICATIONS | |
| 4732.0600 | REPORTS OF THEFT OR LOSS OF RADIATION-PRODUCING EQUIPMENT. |
| 4732.0610 | REPORTS OF MEDICAL EVENTS OR INCIDENTS INVOLVING RADIATION-PRODUCING EQUIPMENT. |
| 4732.0620 | WARNING AND CONTROL DEVICES FOR HIGH AND VERY HIGH RADIATION AREAS. |
| 4732.0630 | BYPASSING A SAFETY DEVICE. |
| CALIBRATIONS AND MEASUREMENT INSTRUMENTS | |
| 4732.0700 | CALIBRATIONS. |
| 4732.0710 | RADIATION SURVEY OR MEASUREMENT INSTRUMENTS. |
| EQUIPMENT REQUIREMENTS | |
| 4732.0800 | GENERAL EQUIPMENT REQUIREMENTS FOR ALL DIAGNOSTIC RADIATION-PRODUCING SYSTEMS. |
| 4732.0820 | GENERAL PURPOSE DIAGNOSTIC RADIATION-PRODUCING EQUIPMENT MANUFACTURED BEFORE 1973. |
| 4732.0825 | FLUOROSCOPIC X-RAY SYSTEMS EXCEPT RADIATION THERAPY SIMULATORS. |
| 4732.0830 | FLUOROSCOPIC DOSE-AREA-PRODUCT MONITOR. |
| 4732.0835 | REQUIREMENTS FOR COMPUTED RADIOGRAPHY, DIGITAL RADIOGRAPHY, OR PHOTOSTIMULABLE STORAGE PHOSPHOR RADIATION-PRODUCING EQUIPMENT. |
| 4732.0850 | BONE DENSITOMETRY SYSTEMS. |
| 4732.0860 | COMPUTED TOMOGRAPHY REQUIREMENTS. |
| 4732.0865 | COMPUTERIZED TOMOGRAPHY DESIGNED FOR VISUALIZATION OF THE HEAD AND SOFT TISSUE OF THE NECK. |
| 4732.0870 | REQUIREMENTS FOR STEREOTACTIC MAMMOGRAPHIC EQUIPMENT. |
| 4732.0875 | VETERINARY MEDICAL RADIOGRAPHIC SYSTEMS. |
| 4732.0880 | INTRAORAL DENTAL RADIOGRAPHIC SYSTEMS. |
| 4732.0890 | EXTRAORAL DENTAL SYSTEMS. |
| 4732.0895 | DENTAL COMPUTED TOMOGRAPHY SYSTEMS. |
| RADIATION THERAPEUTIC REQUIREMENTS | |
| 4732.0900 | GENERAL REQUIREMENTS FOR FACILITIES USING ACCELERATORS. |
| 4732.0925 | GENERAL REQUIREMENTS FOR THERAPEUTIC EQUIPMENT. |
| 4732.0930 | THERAPEUTIC RADIATION MACHINES OF LESS THAN 500 KV. |
| 4732.0940 | THERAPEUTIC RADIATION MACHINES - PHOTON THERAPY SYSTEMS (500 KV AND ABOVE) AND ELECTRON THERAPY SYSTEMS (500 KEV AND ABOVE). |
| 4732.1000 | REQUIREMENTS FOR X-RAY FLUORESCENT ANALYZERS AND BOMB DETECTION UNITS. |
| 4732.1040 | INDUSTRIAL FACILITY REQUIREMENTS FOR USING RADIATION-PRODUCING EQUIPMENT IN MANUFACTURING PROCESSES, GAUGES, AND CABINETS. |
| 4732.1050 | REQUIREMENTS FOR PERMANENT INDUSTRIAL RADIOGRAPHIC INSTALLATIONS. |
| 4732.1055 | INDUSTRIAL RADIOGRAPHIC OPERATING AND EMERGENCY PROCEDURES. |
| 4732.1058 | INDUSTRIAL RADIOGRAPHY IN A TEMPORARY JOB SITE. |
| 4732.1060 | INSTRUCTION AND TRAINING FOR INDUSTRIAL RADIOGRAPHY. |
| 4732.1063 | WARNING DEVICES FOR INDUSTRIAL RADIOGRAPHY FACILITIES. |
| 4732.1065 | POSTING REQUIREMENTS FOR INDUSTRIAL RADIOGRAPHY. |
| 4732.1067 | SURVEILLANCE FOR INDUSTRIAL RADIOGRAPHY. |
| 4732.1070 | RADIOGRAPHER CERTIFICATION. |
| 4732.1100 | INSTALLATION CALIBRATION TESTS AND EQUIPMENT PERFORMANCE TESTS FOR A QUALITY ASSURANCE PROGRAM. |
| 4732.1120 | THERAPEUTIC EQUIPMENT PERFORMANCE TESTS AND LIMITS FOR MEASUREMENT EQUIPMENT. |
| 4732.1130 | EQUIPMENT PERFORMANCE TESTS FOR EXTERNAL BEAM TELETHERAPY AND SIMULATION SYSTEMS. |
4732.0100 PURPOSE AND SCOPE.
Subpart 1.
Purpose.
The purpose of this chapter is to control and prevent hazards to health and safety from ionizing radiation without limiting or interfering with its constructive uses.
Subp. 2.
Scope.
Except as otherwise specified, this chapter applies to all persons who receive, possess, use, transfer, own, or acquire any radiation-producing equipment. The scope of this chapter does not include those sources of ionizing radiation known as radioactive materials, which are covered under chapter 4731.
Subp. 3.
Additional requirements.
In addition to the requirements established in this chapter, the commissioner must impose upon any registrant any requirements deemed appropriate or necessary to minimize danger to public health and safety.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0110 DEFINITIONS.
Subpart 1.
Scope.
For purposes of this chapter, the terms in this part have the meanings given them.
Subp. 2.
Absorbed dose.
"Absorbed dose" means the energy imparted by ionizing radiation per unit mass of irradiated material. The special unit of absorbed dose is the rad under the conventional system of measurement and is the gray under the SI system of measurement.
Subp. 3.
Absorbed dose rate.
"Absorbed dose rate" means absorbed dose per unit time for machine with timers, or dose-monitor unit per unit time for linear accelerators.
Subp. 4.
Accelerator.
"Accelerator" means any machine capable of accelerating electrons, protons, deuterons, or other charged particles in a vacuum and of discharging the resultant particulate or other radiation into a medium at energies usually in excess of 1 MeV. For purposes of this definition, linear accelerator, particle accelerator, and cyclotron are equivalent terms.
Subp. 5.
Added filtration.
"Added filtration" means filtration that is in addition to the inherent filtration.
Subp. 7.
Air kerma (K).
"Air kerma (K)" means the kinetic energy released in air by ionizing radiation. Kerma is determined as the quotient of dE by dM, where dE is the sum of the initial kinetic energies of all the charged ionizing particles liberated by uncharged ionizing particles in air of mass dM. The special name for the unit of kerma is the gray (Gy). The SI unit is joule per kilogram.
Subp. 8.
Aluminum equivalent.
"Aluminum equivalent" means the thickness of type 1100 aluminum alloy affording the same attenuation, under specified conditions, as the material in question.
Subp. 9.
Annual.
"Annual" means an activity is done or is performed at intervals not to exceed 12 months.
Subp. 10.
Appropriate limit or appropriate limits.
"Appropriate limit" or "appropriate limits" means the maximum permissible dose or doses of radiation that may be administered to the whole body or a given part of a human being.
Subp. 11.
As low as reasonably achievable or ALARA.
"As low as reasonably achievable" or "ALARA" means making every reasonable effort to maintain exposure to radiation as far below the dose limits as is practical, consistent with the purpose for which the registered activity is undertaken, taking into account the state of technology, the economics of improvement in relation to benefits to the public health and safety, and other societal and socioeconomic considerations.
Subp. 12.
Attenuation.
"Attenuation" means the reduction of exposure rate upon passage of radiation through matter.
Subp. 13.
Attenuation block.
"Attenuation block" means a block or stack, having dimensions 20 centimeters or larger by 20 centimeters or larger by 3.8 centimeters, of type 1100 aluminum alloy or other materials having equivalent attenuation that is large enough to intercept the entire x-ray beam.
Subp. 14.
Audit.
"Audit" means a planned and documented activity performed according to procedures to determine, by examination and evaluation of objective evidence, the adequacy of and extent to which applicable elements of the quality assurance program have been developed, documented, and effectively implemented.
Subp. 15.
Automatic exposure control or AEC.
"Automatic exposure control" or "AEC" means a device that automatically controls one or more technique factors in order to obtain a required quantity of radiation at a preselected location or locations.
Subp. 16.
Base plus fog density.
"Base plus fog density" means the optical density of a film due to its base density plus any action of the developer on the unexposed silver halide crystals.
Subp. 17.
Beam axis.
"Beam axis" means a line from the source through the centers of the x-ray fields, or for therapy the axis of rotation of the beam-limiting device.
Subp. 18.
Beam-limiting device or BLD.
"Beam-limiting device" or "BLD" means a device used to restrict the dimensions of the x-ray field or useful beam.
Subp. 19.
Beam-monitoring system.
"Beam-monitoring system" means a system designed and installed to detect and measure the radiation present in the useful beam.
Subp. 20.
Beam-scattering filter or foil.
"Beam-scattering filter" or "foil" means a thin piece of material, usually metallic, placed in the beam to scatter a beam of electrons in order to provide a more uniform electron distribution in the useful beam.
Subp. 21.
Bent beam linear accelerator.
"Bent beam linear accelerator" means a linear accelerator geometry in which the accelerated electron beam must change direction by passing through a bending magnet.
Subp. 22.
Bone densitometry system.
"Bone densitometry system" means a medical device that uses electronically produced ionizing radiation to determine the density of bone structures of human patients.
Subp. 23.
C-arm system.
"C-arm system" means an x-ray system in which the image receptor and the x-ray tube housing assembly are connected by a common mechanical support system to maintain a desired spatial relation.
Subp. 24.
Cabinet x-ray system.
"Cabinet x-ray system" means an x-ray system with the x-ray tube installed in an enclosure independent of existing architectural structure except the floor on which it may be placed. The cabinet x-ray system is intended to:
C.
exclude personnel from its interior during generation of radiation.
Included are all x-ray systems designed primarily for the inspection of carry-on baggage at airline, railroad, and bus terminals and in similar facilities. An x-ray tube used within a shielded part of a building or x-ray equipment that may temporarily or occasionally incorporate portable shielding is not considered a cabinet x-ray system.
Subp. 25.
Calibration.
"Calibration" means:
A.
the determination of the response or reading of an instrument relative to a series of known radiation values over the range of the instrument;
B.
the determination of the radiation dose or exposure rate at a designated distance from a radiation source under specified conditions of measurement;
C.
to check, adjust, or systematically standardize to graduations of a quantitative measuring instrument; and
D.
to check, adjust, or systematically bring radiation-producing equipment into manufacturer's specifications.
Subp. 26.
Cephalometric device.
"Cephalometric device" means a device intended for the radiographic visualization and measurement of the dimensions of the human head.
Subp. 27.
Certified cabinet x-ray system.
"Certified cabinet x-ray system" means an x-ray system that has been certified according to Code of Federal Regulations, title 21, section 1010.2, as being manufactured and assembled pursuant to Code of Federal Regulations, title 21, section 1020.40.
Subp. 28.
Certified components.
"Certified components" means components of x-ray systems that are subject to the x-ray equipment performance standards adopted under Public Law 90-602, the Radiation Control for Health and Safety Act of 1968.
Subp. 29.
Certified system.
"Certified system" means an x-ray system that has one or more certified components.
Subp. 30.
Changeable filters.
"Changeable filters" means any filter, exclusive of inherent filtration, that can be removed from the useful beam through any electronic, mechanical, or physical process.
Subp. 31.
Clinical range.
"Clinical range" means the range of control console technique settings that a facility would use in its routine x-ray projections. Equipment performance tests are performed over clinical ranges.
Subp. 32.
Coefficient of variation or C.
"Coefficient of variation" or "C" means the standard deviation divided by the average of the parameters measured.
Subp. 33.
Collimation.
"Collimation" means the restriction of the useful beam to an appropriate area.
Subp. 34.
Collimator.
"Collimator" means a device used to limit the size, shape, and direction of the primary beam.
Subp. 36.
Computed radiography.
"Computed radiography" means a system of creating digital radiographic images that utilizes a storage-phosphor plate instead of film in a cassette. Once the plate is exposed, a laser beam scans it to produce the digital data that is translated into an image.
Subp. 37.
Computed tomography or CT.
"Computed tomography" or "CT" means the production of a tomogram by the acquisition and computer processing of x-ray transmission data.
Subp. 38.
Control panel.
"Control panel" means the part of the x-ray control upon which the switches, knobs, push buttons, and other hardware necessary for manually setting the technique factors are mounted.
Subp. 39.
CT conditions of operation.
"CT conditions of operation" means all selectable parameters governing the operation of a CT system including, but not limited to, nominal tomographic section thickness, filtration, and the technique factors defined in subpart 195.
Subp. 40.
CT dose index or CTDI.
"CT dose index" or "CTDI" means the integral from minus 7T to plus 7T of the dose profile along a line perpendicular to the tomographic plane divided by the product of the nominal tomographic section thickness (T) and the number of tomograms produced in a single scan (n), that is:
| CTDI | = | 1/nT | -7T∫+7T | D(z) | dz |
where:
z = position along a line perpendicular to the tomographic plane;
D(z) = dose at position z;
T = nominal tomographic section thickness; and
n = number of tomograms produced in a single scan.
This definition assumes that the dose profile is centered around z=0 and that, for a multiple tomogram system, the increment of adjacent scans is nT.
Subp. 41.
CT gantry.
"CT gantry" means the tube housing assemblies, beam-limiting devices, and detectors, as well as the supporting structures and frames that hold those components.
Subp. 42.
CT number.
"CT number" means the number used to represent the x-ray attenuation associated with each elemental area of the CT image.
Subp. 43.
CT scan.
"CT scan" means the complete process of collecting x-ray transmission data for the production of a tomogram. This includes data collected simultaneously during a single scan for the production of one or more tomogram.
Subp. 44.
CT scan increment.
"CT scan increment" means the amount of relative displacement of the patient with respect to the CT system between successive scans measured along the direction of the displacement.
Subp. 45.
CT scan time.
"CT scan time" means the time between the beginning and end of x-ray transmission data accumulation for a CT scan.
Subp. 46.
Dead-man switch.
"Dead-man switch" means a switch so constructed that a circuit-closing contact can be maintained only by continuous pressure on the switch by the operator.
Subp. 47.
Declared pregnant woman.
"Declared pregnant woman" means a woman who has voluntarily informed the registrant, in writing, of her pregnancy and the estimated date of conception. The declaration remains in effect until the declared pregnant woman withdraws the declaration in writing or is no longer pregnant.
Subp. 48.
Densitometer.
"Densitometer" means an instrument that measures the degree of blackening or radiographic density of a film due to radiation or light by measuring the ratio of the light intensity incident on the film to the light intensity transmitted by the film.
Subp. 49.
Diagnostic radiological physicist.
"Diagnostic radiological physicist" means an individual who is qualified to practice independently in the appropriate subfields for medical diagnostic physics and is:
A.
certified in radiological physics or diagnostic radiological physics by the American Board of Radiology;
D.
a holder of a masters degree in medical physics, radiological sciences, or an equivalent field involving graduate study in physics applied to the application of radiation to humans from an accredited college or university and has at least two years of full-time practical training or supervised experience under an individual who meets the qualifications in item A, B, or C.
Subp. 50.
Diagnostic x-ray imaging system.
"Diagnostic x-ray imaging system" means an assemblage of components for the generation, emissions, and reception of x-rays and the transformation, storage, and visual display of the resultant x-ray image which are designed and used for irradiation of any part of a body for the purpose of diagnosis or visualization.
Subp. 51.
Digital radiography.
"Digital radiography" means a radiographic image displayed on a video monitor after computer processing.
Subp. 52.
Direct supervision.
"Direct supervision" means guidance and instruction by a qualified individual who is physically present and watching the performance of the radiological operation or procedure and in such proximity that contact can be maintained and immediate assistance can be given as required.
Subp. 53.
Dose.
"Dose" means absorbed radiation dose, radiation dose equivalent, effective radiation dose equivalent, committed radiation dose equivalent, committed effective radiation dose equivalent, or total effective radiation dose equivalent. For purposes of this chapter, "radiation dose" is an equivalent term.
Subp. 54.
Dose equivalent or DE.
"Dose equivalent" or "DE" means a quantity used for radiation protection purposes that expresses on a common scale for all radiations the irradiation incurred by exposed persons. It is defined as the product of the absorbed radiation dose and the quality factor. For x-rays and gamma rays, the dose equivalent in rem is usually assumed to be numerically equal to either the exposure in roentgens or the absorbed dose in rad. The special unit radiation dose equivalent is the rem under the conventional measurement system and is the sievert under the SI measurement system.
Subp. 55.
Dose limits or limits.
"Dose limits" or "limits" means the permissible upper bounds of radiation doses.
Subp. 56.
Dose-monitoring system.
"Dose-monitoring system" means a system of devices for the detection, measurement, and display of quantities of radiation that can be related to the absorbed dose at a given location within a defined geometry.
Subp. 57.
Dose-monitor unit.
"Dose-monitor unit" means a unit response from the dose-monitoring system from which the absorbed radiation dose has been calculated.
Subp. 58.
Effective dose equivalent or HE.
"Effective dose equivalent" or "HE" means the sum of the products of the dose equivalent to each organ or tissue (HT) and the weighting factor (wT) applicable to each of the body organs or tissues that are irradiated.
Subp. 59.
Electron-beam generator.
"Electron-beam generator" means a type of electron accelerator in which the electron beam is brought out into the atmosphere for irradiation purposes.
Subp. 60.
Electronic signature.
"Electronic signature" means an electronic sound, symbol, or process attached to or logically associated with a record, and executed or adopted by a person with the intent to sign the record according to Minnesota Statutes, chapter 325L.
Subp. 61.
Exposure.
"Exposure" means being exposed to ionizing radiation. The unit of exposure is the Roentgen in air (R). The SI unit is 2.58 x 10-4 coulombs per kilogram.
Subp. 62.
Exposure rate.
"Exposure rate" means the exposure per unit of time, such as roentgen per minute, milliroentgen per hour. The SI unit is 10-4 coulombs per kilogram per hour.
Subp. 63.
External beam radiation therapy.
"External beam radiation therapy" means therapeutic irradiation in which the source of radiation is at a distance from the body.
Subp. 64.
Facility.
"Facility" means the location at which one or more sources of radiation are installed or located within one building, one vehicle, at one address, and are under the same administrative control.
Subp. 65.
Field emission equipment.
"Field emission equipment" means equipment that uses an x-ray tube in which electron emission from the cathode is due solely to the action of an electric field.
Subp. 66.
Field-flattening filter.
"Field-flattening filter" means a filter used to homogenize the absorbed dose rate over the radiation field.
Subp. 67.
Filmless radiography or photostimulable storage phosphor (PSP) imaging.
"Filmless radiography" or "photostimulable storage phosphor (PSP) imaging" means a system that could employ reusable imaging plates, associated hardware and software to acquire and display digital projection radiographs. These imaging devices are known by a number of names including computed radiography (CR), photostimulable storage phosphor (PSP) imaging, or digital radiography (DR). In the digital form, PSP images are readily put into picture archiving and communications systems and viewed on a monitor rather than viewing an image on x-ray film.
Subp. 68.
Filter or filtration.
"Filter" or "filtration" means material placed in the useful beam to preferentially absorb selected radiations.
Subp. 69.
Fluoroscopic imaging assembly.
"Fluoroscopic imaging assembly" means a subsystem in which x-ray photons produce a set of fluoroscopic or radiographic recorded images from the fluoroscopic image receptor. Fluoroscopic imaging assembly includes image receptors such as the image intensifier and spot-film device, electrical interlocks, if any, and structural material providing linkage between the image receptor and diagnostic source assembly.
Subp. 70.
Focal spot.
"Focal spot" means the area of the anode of the x-ray tube bombarded by the electrons accelerated from the cathode and from which the useful beam originates.
Subp. 71.
Gantry.
"Gantry" means the part of the system supporting and allowing possible movements of the radiation head.
Subp. 72.
General purpose radiographic x-ray system.
"General purpose radiographic x-ray system" means a radiographic x-ray system that, by design, is not limited to radiographic examination of specific anatomical regions.
Subp. 74.
Gray or Gy.
"Gray" or "Gy" means the unit of absorbed radiation dose equal to one joule per kilogram. The conventional system equivalent is 100 rad.
Subp. 75.
Half-value layer or HVL.
"Half-value layer" or "HVL" means the thickness of a specified material that attenuates the beam of radiation to such an extent that the exposure rate is reduced to one-half of its original value. The contribution of all scattered radiation, other than any that might be present initially in the beam concerned, is considered excluded.
Subp. 76.
Healing arts.
"Healing arts" means health professions for diagnostic or healing treatment of human and animal maladies that are regulated under Minnesota Statutes, chapter 147, 153, or 156; or section 148.01, 148.106, or 150A.05, subdivision 1, clause (4), for the lawful practice of medicine, dentistry, veterinary medicine, osteopathic medicine, chiropractic, and podiatry.
Subp. 77.
Healing arts screening or screening.
"Healing arts screening" or "screening" means the testing of individuals with x-ray equipment to detect or evaluate health conditions when the tests are not specifically and individually ordered by a licensed practitioner of the healing arts who is legally authorized to prescribe the tests for the purpose of diagnosis or treatment.
Subp. 78.
High radiation area.
"High radiation area" means any area, accessible to individuals, in which radiation levels from radiation sources external to the body could result in an individual receiving a radiation dose equivalent in excess of 0.1 rem (1.0 mSv) in one hour at 30 centimeters from any source of radiation or 30 centimeters from any surface that the radiation penetrates.
Subp. 79.
Image intensifier.
"Image intensifier" means a device, installed in its housing, that instantaneously converts an x-ray pattern into a corresponding light image of higher energy intensity.
Subp. 80.
Image quality.
"Image quality" means the overall clarity and detail of a radiographic image. Limiting spatial resolution (or resolving power), image sharpness, and image contrast are three common measures of image quality.
Subp. 81.
Image receptor.
"Image receptor" means a device such as a fluorescent screen or radiographic film, solid-state detector, or gaseous detector that transforms incident x-ray photons either into a visible image or into another form that can be made into a visible image by further transformations.
Subp. 83.
Individual monitoring.
"Individual monitoring" means the assessment of dose equivalent by the use of individual monitoring devices or by the use of radiation survey data.
Subp. 84.
Individual monitoring devices.
"Individual monitoring devices" means devices designed to be worn by a single individual for the assessment of dose equivalent. For purposes of this chapter, "personal dosimeter" and "dosimeter" are equivalent terms. Examples of individual monitoring devices are film badges, thermoluminescent devices, pocket ionization chambers, and optically stimulated luminescence devices.
Subp. 85.
Industrial cabinet baggage system.
"Industrial cabinet baggage system" has the meaning given for cabinet x-ray systems in subpart 24.
Subp. 86.
Industrial vault radiography.
"Industrial vault radiography" means industrial radiography conducted in an enclosure, shielded so that radiation levels at every location on the exterior meet the unrestricted limitations in this chapter.
Subp. 87.
Industrial radiographer.
"Industrial radiographer" means any individual who performs or who, in attendance at the site where ionizing radiation sources are being used, personally supervises industrial radiographic operations and who is responsible to the registrant for ensuring compliance with this chapter.
Subp. 88.
Industrial radiographer's assistant.
"Industrial radiographer's assistant" means an individual who uses radiographic exposure devices or radiation survey instruments in industrial radiography under the supervision of an industrial radiographer.
Subp. 89.
Industrial radiography.
"Industrial radiography" means an examination of the structure of materials by the nondestructive methods of utilizing ionizing radiation to make images. Industrial radiography does not include cabinet x-ray or the use of ionizing radiation-producing equipment to measure thickness, to identify levels and material in containers, or to analyze the chemical compositions. Industrial x-ray does not include the use of ionizing radiation-producing equipment in forensic, medical, or veterinary research.
Subp. 90.
Inherent filtration.
"Inherent filtration" means the filtration of the useful beam provided by the permanently installed components of the tube housing assembly.
Subp. 91.
Inspection.
"Inspection" means an official examination or observation, including but not limited to tests, radiation surveys, and monitoring to determine compliance with rules, regulations, and requirements of the commissioner.
Subp. 92.
Instrument traceability.
"Instrument traceability" for ionizing radiation measurements means the ability to show that an instrument has been calibrated at specified time intervals using a national standard or a transfer standard. If a transfer standard is used, the calibration must be at a laboratory accredited by a program that requires continuing participation in measurement quality assurance with the National Institute of Standards and Technology (NIST), or other equivalent national or international programs.
Subp. 93.
Interlock.
"Interlock" means a device that automatically causes a reduction of the exposure rate upon entry by personnel into a high radiation area. An interlocking device must prevent the start or continued operation of equipment unless certain predetermined conditions prevail.
Subp. 94.
Ionizing radiation.
"Ionizing radiation" means any radiation capable of producing displacing electrons from atoms or molecules, thereby producing ions. Examples: alpha, beta, gamma, x-ray, and neutron radiation.
Subp. 95.
Irradiation.
"Irradiation" means the exposure of a living being or matter to ionizing radiation.
Subp. 96.
Isocenter.
"Isocenter" means a fixed point in space through which pass the central axes of radiation beams for all possible beam orientations and field sizes.
Subp. 97.
Kilovolt peak or kVp.
"Kilovolt peak" or "kVp" has the meaning given for peak tube potential in subpart 120.
Subp. 98.
Lead equivalence or lead equivalent.
"Lead equivalence" or "lead equivalent" means the thickness of lead affording the same attenuation, under specified conditions, as the material in question.
Subp. 99.
Leakage radiation.
"Leakage radiation" means radiation emanating from the radiation source assembly except for the useful beam and radiation produced when the exposure switch or timer is not activated.
Subp. 100.
Leakage technique factors.
"Leakage technique factors" means the technique factors associated with the diagnostic or therapeutic source assembly that are used in measuring leakage radiation.
Subp. 101.
Licensed practitioner of the healing arts.
"Licensed practitioner of the healing arts" means health professionals for diagnostic or healing treatment of human and animal maladies, which are licensed under Minnesota Statutes, chapter 147, 153, or 156; or section 148.01, 148.106, or 150A.05, subdivision 1, clause (4), for the lawful practice of medicine, dentistry, veterinary medicine, osteopathic medicine, chiropractic, and podiatry.
Subp. 102.
Light field.
"Light field" means the area of the intersection of the light beam from the beam-limiting device and one of the set of planes parallel to and including the plane of the image receptor whose perimeter is the locus of points at which the illumination is one-fourth of the maximum in the intersection.
Subp. 103.
Line-voltage regulation.
"Line-voltage regulation" means the difference between the no-load and the load line potentials expressed as a percent of the load line potential. It is calculated using the following equation:
Percent line-voltage regulation = 100 (Vn - V1)/V1
| where: |
| Vn = no-load line potential; and |
| V1 = load line potential. |
Subp. 106.
Maximum line current.
"Maximum line current" means the root-mean-square current in the supply line of an x-ray system operating at its maximum rating.
Subp. 107.
Medical event.
"Medical event" means the administration of radiation received from radiation-producing equipment and includes:
A.
therapeutic administration involving:
(3)
a dose to tissue other than the treatment site that is 50 percent or more of the dose expected from the administration defined in the written directive;
(5)
a total radiation dosage delivered that differs from the prescribed dosage by 20 percent or more or falls outside the prescribed dosage range; or
(6)
a fractionated radiation dose delivered that differs from the prescribed dose, for a single fraction, by 50 percent or more; and
Subp. 108.
Medical particle accelerator.
"Medical particle accelerator" has the meaning given for accelerator in subpart 4.
Subp. 109.
Medical physicist.
"Medical physicist" has the meaning given for diagnostic radiological physicist in subpart 49, or therapeutic radiological physicist in subpart 200.
Subp. 110.
Medical uses.
"Medical uses" means the intentional internal or external administration of radiation to human and animal patients or human research subjects.
Subp. 111.
Megavolt (MV) or mega electron volt (MeV).
"Megavolt," "MV," or "mega electron volt," "MeV," means the energy equal to that acquired by a particle with one electron charge in passing through a potential difference of 1,000,000 volts in a vacuum. Current convention is to use MV for photons and MeV for electrons.
Subp. 112.
Moving beam radiation therapy.
"Moving beam radiation therapy" means radiation therapy with continuous displacement of one or more mechanical axes relative to the patient during irradiation. It includes arc therapy, skip therapy, conformal therapy, and rotational therapy.
Subp. 113.
Nominal tomographic section thickness.
"Nominal tomographic section thickness" means the full width at half-maximum at the center of the cross-sectional volume over which x-ray transmission data are collected.
Subp. 114.
Nominal treatment distance.
"Nominal treatment distance" means:
A.
for electron irradiation, the distance from the scattering foil, virtual source, or exit window of the electron beam to the entrance surface of the irradiated object along the central axis of the useful beam;
B.
for x-ray irradiation, the virtual source or target to isocenter distance along the central axis of the useful beam; and
Subp. 115.
Nonstochastic effects.
"Nonstochastic effects" means health effects the severity of which varies with the radiation dose, and for which a threshold is believed to exist. Radiation-induced cataract formation is an example of a nonstochastic effect.
Subp. 116.
Occupational dose.
"Occupational dose" means the dose received by an individual in the course of employment in which the individual's assigned duties for the registrant involve exposure to radiation-producing equipment, whether or not the radiation-producing equipment is in the possession of the registrant. Occupational dose does not include doses received from background radiation, from any medical administration the individual has received, from exposure to individuals administered radioactive material and released in accordance with chapter 4731, from voluntary participation in medical research programs, or as a member of the public.
Subp. 117.
Open-beam configuration.
"Open-beam configuration" means an analytical x-ray system in which an individual could accidentally place some part of the body in the primary beam or secondary scattered beam path during normal operation.
Subp. 118.
Optical density or O.D.
"Optical density" or "O.D." means the logarithm of the incident light intensity minus the logarithm of the transmitted light intensity.
Subp. 119.
Patient.
"Patient" means an individual or animal subjected to healing arts examination, diagnosis, or treatment.
Subp. 120.
Peak tube potential.
"Peak tube potential" means the maximum value of the potential difference across the x-ray tube during an exposure.
Subp. 121.
Permanent radiographic installation.
"Permanent radiographic installation" means a shielded enclosed room, cell, vault, or structure that is not moved and is not located at a temporary job site. The installation is designed or intended for radiography, and in which radiography is regularly performed.
Subp. 122.
Person.
"Person" means any individual, corporation, partnership, firm, association, trust, estate, public or private institution, group, agency, political subdivision of this state, and any legal successor, representative, agent or agency of the foregoing, excluding federal government agencies.
Subp. 123.
Personal protective garments.
"Personal protective garments" mean garments, including aprons, gloves, and thyroid collars made of radiation absorbing materials used to reduce radiation exposure.
Subp. 124.
Personal monitoring dosimeter.
"Personal monitoring dosimeter" has the meaning given for individual monitoring devices in subpart 84.
Subp. 125.
Phantom.
"Phantom" means a volume of material behaving in a manner similar to tissue with respect to the attenuation and scattering of radiation.
Subp. 126.
Phototimer.
"Phototimer" means a method for controlling radiation exposures to image receptors by measuring the amount of radiation that reaches a radiation monitoring device. A radiation monitoring device is part of an electronic circuit that controls the duration of time the x-ray tube is activated. "Phototimer" includes the meaning given for automatic exposure control in subpart 15.
Subp. 126a.
Physician assistant.
"Physician assistant" means a person registered according to Minnesota Statutes, chapter 147A, who is qualified by academic, practical training, or both to provide patient services as specified in the physician-physician assistant agreement recognized by the Minnesota Board of Medical Practice.
Subp. 127.
Pixel or picture element.
"Pixel" or "picture element" means an elemental area of a digital image.
Subp. 128.
Port film or portal imaging.
"Port film" or "portal imaging" means a radiographic film or electronic image taken with a therapeutic x-ray system to verify proper setup of the treatment field.
Subp. 129.
Positive beam limiting or limitation or PBL.
"Positive beam limiting or limitation" or "PBL" means the automatic or semiautomatic adjustment of an x-ray beam to the size of the selected image receptor, whereby exposures cannot be made without this adjustment.
Subp. 130.
Position-indicating device or PID.
"Position-indicating device" or "PID" means a device on dental x-ray equipment used to indicate the beam position and to establish the source-to-skin distance.
Subp. 131.
Prescribed dose.
"Prescribed dose" means the total radiation dose and radiation dose per fraction as documented in the written directive or therapeutic order.
Subp. 132.
Primary beam.
"Primary beam" means radiation that passes through an aperture of the source housing by a direct path from the x-ray tube located in the radiation-producing equipment housing.
Subp. 133.
Primary dose-monitoring system.
"Primary dose-monitoring system" means a system that will monitor the useful beam during irradiation and will terminate irradiation when a preselected number of dose monitor units have been acquired.
Subp. 134.
Primary protective barrier.
"Primary protective barrier" means the material, excluding filters, placed in the useful beam for protection purposes to reduce the radiation exposure.
Subp. 136.
Protective barrier or barrier.
"Protective barrier" or "barrier" means a barrier of radiation absorbing materials used to reduce radiation exposure.
Subp. 138.
Pulsed mode.
"Pulsed mode" means operation of an x-ray system so that the x-ray tube current is pulsed by the x-ray control to produce one or more exposure intervals of less than one-half second duration.
Subp. 139.
Quality assurance program.
"Quality assurance program" means an all-encompassing program including quality control that extends to administrative, education, and preventive maintenance methods. It includes a continuing evaluation of the adequacy and effectiveness of the overall imaging program, with a view to initiating corrective measures when necessary. The nature and extent of this program will vary with the size and type of the facility, and the type of activities conducted.
Subp. 140.
Quality control.
"Quality control" means a series of distinct technical procedures that ensure the production of a satisfactory product. Its aim is to provide quality that is not only satisfactory but also dependable and economic. The quality control procedures are concerned directly with the equipment.
Subp. 144.
Radiation area.
"Radiation area" means an area accessible to individuals in which the radiation levels could result in an individual receiving a dose equivalent in excess of 0.005 rem (0.05 mSv) in one hour at 30 centimeters from the source of radiation or from any surface that the radiation penetrates.
Subp. 145.
Radiation detector or detector.
"Radiation detector" or "detector" means a device that in the presence of radiation provides a signal or other indication suitable for use in measuring one or more quantities of incident radiation.
Subp. 146.
Radiation head.
"Radiation head" means the structure from which the useful beam emerges.
Subp. 147.
Radiation-producing equipment.
"Radiation-producing equipment" means any device capable of producing radiation.
Subp. 148.
Radiation protection.
"Radiation protection" means the use of time, distance, shielding, and other personnel protective garments.
Subp. 149.
Radiation safety officer.
"Radiation safety officer" means an individual who has the knowledge and training to apply appropriate radiation protection standards, and has been assigned such responsibility by the registrant.
Subp. 150.
Radiation therapy simulation system.
"Radiation therapy simulation system" means a radiographic, fluoroscopic, or CT x-ray system including all software applicable to the process intended for localizing the volume to be exposed during radiation therapy and confirming the position and size of the therapeutic irradiation field.
Subp. 151.
Radiograph.
"Radiograph" means an image produced on a radiosensitive surface, such as a photographic film or digital plate, by radiation other than visible light, such as by x-rays passed through an object or by photographing a fluoroscopic image that results in a permanent record.
Subp. 152.
Radiographic imaging system.
"Radiographic imaging system" means any system where a permanent or semipermanent image is recorded on an image receptor by the action of ionizing radiation.
Subp. 152a.
Radiology practitioner assistant or RPA.
"Radiology practitioner assistant" or "RPA" means an individual who is an advanced level radiographer registered with the American Registry of Radiologic Technologists and certified by the Certification Board for Radiology Practitioner Assistants. The individual is qualified by completion of an educational program recognized by the Board of Directors of the Certification Board for Radiology Practitioner Assistants. The RPA may provide patient services as specified in an agreement with a supervising radiologist.
Subp. 153.
Rated line voltage.
"Rated line voltage" means the range of potentials, in volts, of the supply line specified by the manufacturer at which the radiation-producing equipment is designed to operate.
Subp. 154.
Rating.
"Rating" means the operating limits as specified by the component manufacturer.
Subp. 155.
Recording.
"Recording" means producing a retrievable form of an image resulting from x-ray photons.
Subp. 156.
Reference man.
"Reference man" means a hypothetical aggregation of human physical and physiological characteristics. These characteristics may be used by researchers and public health workers to standardize results of experiments and to relate biological insult to a common base.
Subp. 157.
Reference plane.
"Reference plane" means a plane that is displaced from and parallel to the tomographic plane.
Subp. 159.
Registered radiologist assistant or RRA.
"Registered radiologist assistant" or "RRA" means a person who is an advanced level radiographer certified and registered in radiography by the American Registry of Radiologic Technologists and has successfully completed all elements of a radiologist assistant educational program recognized by the ARRT. The RRA would be able to provide patient services as specified in an agreement with a supervising radiologist.
Subp. 160.
Registrant.
"Registrant" means:
A.
a person having administrative control of any radiation-producing equipment except those specifically exempted under this chapter and who is legally obligated to register with the commissioner according to this chapter; or
Subp. 161.
Registration.
"Registration" means registration with the commissioner according to this chapter.
Subp. 162.
Rem.
"Rem" means a special unit of dose equivalence. The SI equivalent is 0.01 sievert.
Subp. 163.
Restricted area.
"Restricted area" means any area to which access or egress may be limited by the registrant for purposes of protection of individuals from exposure to radiation.
Subp. 164.
Retake or reject.
"Retake" or "reject" means any diagnostic radiographic imaging that had to be retaken, reexposing the patient to radiation because of some error, failure, or degradation in the radiographic imaging process.
Subp. 165.
Retake or reject analysis program.
"Retake or reject analysis program" means an ongoing analysis of retakes or rejects that provides information about existing imaging problems in a radiology department.
Subp. 166.
Roentgen or R.
"Roentgen" or "R" means a special unit of exposure. The roentgen is equal to 2.58 x 10-4 coulombs per kilogram of air.
Subp. 167.
Scattered radiation or secondary radiation.
"Scattered radiation" or "secondary radiation" means radiation that, during passage through matter, has been deviated in direction and may have also been modified by a decrease in energy.
Subp. 168.
Secondary dose-monitoring system.
"Secondary dose-monitoring system" means a system that will terminate irradiation if the primary dose-monitoring system fails.
Subp. 169.
Secondary protective barrier.
"Secondary protective barrier" means a barrier sufficient to attenuate stray radiation.
Subp. 170.
Sensitometer.
"Sensitometer" means an instrument designed to reproducibly expose a piece of film to a number of different levels of light intensity.
Subp. 171.
Sensitometric strip.
"Sensitometric strip" means a film exposed by a sensitometer, resulting in a gray scale range. The strips are used to measure the range of densities from minimum to maximum.
Subp. 172.
Sensitometry.
"Sensitometry" means a quantitative measurement of the response of film to exposure and development. Sensitometry is used to test the processor setup and stability.
Subp. 173.
Service provider.
"Service provider" means a person engaged in the business of assembling, installing, repairing, or replacing one or more components into diagnostic or industrial radiation-producing equipment system or subsystem or conducting equipment performance evaluations on diagnostic or industrial equipment. Service providers must be registered with the commissioner under part 4732.0275.
Subp. 174.
Shadow tray.
"Shadow tray" means a device attached to the radiation head to support auxiliary beam-limiting material.
Subp. 175.
Shutter.
"Shutter" means a device attached to the tube housing assembly that can totally intercept the useful beam and has a lead equivalency not less than that of the tube housing assembly.
Subp. 176.
SI equivalent.
"SI equivalent" means units that conform to the international system of units.
Subp. 177.
Sievert or Sv.
"Sievert" or "Sv" means the SI unit of any quantities expressed as dose equivalent. The conventional system equivalent is the rem.
Subp. 179.
Source of radiation.
"Source of radiation" means a device or equipment that emits or is capable of producing radiation. For purposes of this chapter, this is equivalent to radiation-producing equipment.
Subp. 180.
Source-to-image distance or SID.
"Source-to-image distance" or "SID" means the distance from the source to the center of the input surface of the image receptor.
Subp. 181.
Source-to-skin distance or SSD.
"Source-to-skin distance" or "SSD" means the distance between the source and the skin of the patient.
Subp. 182.
Spot check.
"Spot check" means a procedure that is performed to ensure that a previous calibration continues to be valid.
Subp. 183.
Spot film.
"Spot film" means a radiograph that is made during a fluoroscopic procedure to permanently record conditions that exist during that fluoroscopic procedure.
Subp. 184.
Spot-film device.
"Spot-film device" means a device intended to transport and position a radiographic image receptor between the x-ray source and fluoroscopic image receptor. Spot-film device includes a device intended to hold a cassette over the input end of the fluoroscopic image receptor to produce a radiograph.
Subp. 185.
Stationary beam therapy.
"Stationary beam therapy" means radiation therapy without relative displacement of the useful beam and the patient during irradiation.
Subp. 186.
Step wedge.
"Step wedge" means a quality control test tool made of type 1100 aluminum with 11 steps.
Subp. 187.
Stepless adjustment.
"Stepless adjustment" means a method of adjusting collimator blades continuously rather than in fixed increments.
Subp. 188.
Stochastic effects.
"Stochastic effects" means health effects that occur randomly and for which the probability of the effect occurring, rather than its severity, is assumed to be a linear function of dose without threshold. Hereditary effects and cancer incidence are examples of stochastic effects.
Subp. 189.
Storage.
"Storage" means a condition in which a device or radiation-producing equipment is not being used for an extended period of time and has been made inoperable.
Subp. 190.
Storage area.
"Storage area" means a location, facility, or vehicle that is locked or has a physical barrier to prevent accidental exposure to, tampering with, or unauthorized removal of the device, container, or source.
Subp. 191.
Stray radiation.
"Stray radiation" means the sum of leakage radiation and scattered radiation.
Subp. 192.
Supervising physician.
"Supervising physician" means a Minnesota licensed physician who accepts full medical responsibility for the performance, practice, and activities of a registered radiologist assistant or a radiology practitioner assistant.
Subp. 193.
Survey or radiation survey.
"Survey" or "radiation survey" means an evaluation of the radiological conditions and potential hazards incident to the use of radiation-producing equipment. When appropriate, such evaluation includes, but is not limited to, tests, physical examinations, and measurements of levels of radiation.
Subp. 194.
Target.
"Target" means the part of an x-ray tube or accelerator onto which a beam of accelerated particles is directed to produce ionizing radiation or other particles.
Subp. 195.
Technique factors.
"Technique factors" means the conditions of operation, specified as follows:
A.
for capacitor energy storage equipment, peak tube potential in kV and quantity of charge in mAs;
B.
for field emission equipment rated for pulsed operation, peak tube potential in kV, and number of x-ray pulses;
C.
for CT x-ray systems designed for pulsed operation, peak tube potential in kV, scan time in seconds, and either tube current in mA, x-ray pulse width in seconds, and the number of x-ray pulses per scan, or the product of milliamperage, x-ray pulse width, and the number of x-ray pulses in mAs;
D.
for CT x-ray systems not designed for pulsed operation, peak tube potential in kV, and either the tube current in mA and scan time in seconds, or the product of milliamperage and exposure time in mAs and the scan time when the scan time and exposure time are equivalent;
E.
for phototimed or automatic exposure controlled equipment, all necessary indicators including anatomical, if applicable, that must be activated before exposure; and
F.
for all other equipment, peak tube potential in kV and either tube current in mA and exposure time in seconds, or the product of milliamperage and exposure time in mAs.
Subp. 196.
Television receiver.
"Television receiver" means an electronic product designed to receive and display a television picture through broadcast, cable, or closed-circuit television.
Subp. 197.
Temporary job site.
"Temporary job site" means a location where radiography is performed, other than a location listed in a registration.
Subp. 198.
Termination of irradiation.
"Termination of irradiation" means the stopping of irradiation in a fashion that will not permit continuance of irradiation without the resetting of operating conditions at the control panel.
Subp. 199.
Therapeutic radiation machine.
"Therapeutic radiation machine" means x-ray or electron-producing equipment designed and used for external beam radiation therapy.
Subp. 200.
Therapeutic radiological physicist.
"Therapeutic radiological physicist" means an individual qualified to practice independently in the subfields for medical therapeutic physics who:
A.
is certified in radiological physics or therapeutic radiological physics by the American Board of Radiology;
C.
is certified in therapeutic radiological physics by the Canadian College of Medical Physics; or
D.
holds a masters degree or doctor's degree in medical physics, radiological sciences, or an equivalent field involving graduate study in physics applied to the application of radiation to humans from an accredited college or university and have at least one year of full-time practical training and experience involving work in a radiation therapy facility under an individual who meets the qualifications in this item or item A, B, or C.
Subp. 201.
Therapeutic-type protective tube housing.
"Therapeutic-type protective tube housing" means the definitions in items A to C.
A.
For x-ray therapy equipment not capable of operating at 500 kilovolt peak (kVp) or above, the following definition applies: an x-ray tube housing so constructed that the leakage radiation at a distance of one meter from the source does not exceed one rad (0.01 Gy) in an hour when the tube is operated at its maximum rated continuous current for the maximum rated tube potential.
B.
For x-ray therapy equipment capable of operation at 500 kilovolt peak (kVp) or above, the following definition applies: an x-ray tube housing so constructed that leakage radiation at a distance of one meter from the source does not exceed either one rad (0.01 Gy) in an hour or 0.1 percent of the useful beam dose rate at one meter from the source, whichever is greater, when the machine is operated at its maximum rated continuous current for the maximum rated accelerating potential.
C.
In either case, small areas of reduced protection are acceptable provided the average reading over any 100 square centimeters area at one meter distance from the source does not exceed the values given in items A and B.
Subp. 203.
Tomographic plane.
"Tomographic plane" means the geometric plane that is identified as corresponding to the output tomogram.
Subp. 204.
Tomographic section.
"Tomographic section" means the volume of an object whose x-ray attenuation properties are imaged in a tomogram.
Subp. 205.
Traceable to a standard.
"Traceable to a standard" means a comparison, either directly or indirectly, to a standard maintained by the National Institute of Standards and Technology (NIST) and that all comparisons have been documented.
Subp. 206.
Tube housing assembly.
"Tube housing assembly" means the tube housing with tube installed. It includes high voltage and filament transformers and other appropriate elements when contained within the tube housing.
Subp. 207.
Tube rating chart.
"Tube rating chart" means the set of curves that specify the rated limits of operation of the tube in terms of the technique factors.
Subp. 208.
Type 1100 aluminum alloy.
"Type 1100 aluminum alloy" means an alloy of aluminum that has a nominal chemical composition of 99 percent minimum aluminum and 0.12 percent copper.
Subp. 209.
Useful beam.
"Useful beam" means the radiation emanating from the tube housing port or the radiation head and passing through the aperture of the beam-limiting device when the exposure controls are in a mode to cause the system to produce radiation.
Subp. 210.
Utilization log.
"Utilization log" means a record of procedures conducted in a certain time frame and following a set of requirements:
Subp. 211.
Variable-aperture beam-limiting device.
"Variable-aperture beam-limiting device" means a beam-limiting device that has a capacity for stepless adjustment of the x-ray field size at a given SID.
Subp. 212.
Very high radiation area.
"Very high radiation area" means an area accessible to individuals, where radiation levels from radiation-producing equipment external to the body could result in an individual receiving an absorbed dose in excess of 500 rad (5 Gy) in one hour at one meter from any surface that the radiation penetrates.
Subp. 213.
Virtual source.
"Virtual source" means a point from which radiation appears to originate.
Subp. 214.
Visible area.
"Visible area" means the portion of the input surface of the image receptor over which incident x-ray photons are producing a visible image.
Subp. 215.
Wedge filter.
"Wedge filter" means an added filter effecting continuous change in transmission on all or part of the useful beam.
Subp. 216.
Worker.
"Worker" means an individual who engages in activities with sources of ionizing radiation that require registration by the commissioner and that are controlled by a registrant.
Subp. 217.
Written directive or written order.
"Written directive" or "written order" means a dated order either in writing or electronically for a specific patient, specific procedure, and has an indication of the licensed practitioner of the healing arts ordering the procedure.
Subp. 218.
X-ray control.
"X-ray control" means a device, switch, or other similar means by which an operator initiates and terminates the radiation exposure. The x-ray exposure control may include associated equipment such as timers and back-up timers.
Subp. 219.
X-ray equipment.
"X-ray equipment" means an x-ray system, subsystem, or component. Types of x-ray equipment are listed in items A to D.
B.
"Portable industrial x-ray equipment" means industrial x-ray equipment designed to be brought to a temporary job site to perform temporary industrial radiography.
C.
"Portable x-ray equipment" means x-ray equipment on wheels or casters and designed to be brought to a patient when the patient's condition does not permit transfer to a fixed location.
D.
"Stationary x-ray equipment" means x-ray equipment installed in a fixed location within a facility.
Subp. 220.
X-ray field.
"X-ray field" means the area of the intersection of the useful beam and any one of the set of planes parallel to and including the plane of the image receptor, whose perimeter is the locus of points at which the exposure rate is one-fourth of the maximum in the intersection.
Subp. 221.
X-ray generator.
"X-ray generator" means a type of electron accelerator in which the electron beam is used mainly for the production of x-rays.
Subp. 222.
X-ray high-voltage generator.
"X-ray high-voltage generator" means a device that transforms electrical energy from the potential supplied by the x-ray control to the tube operating potential. The device may also include means for transforming alternating current to direct current filament transformers for the x-ray tube, high-voltage switches, electrical protective devices, and other appropriate elements.
Subp. 223.
X-ray system.
"X-ray system" means an assemblage of components for the controlled production of x-rays. It includes minimally an x-ray high-voltage generator, an x-ray control, a tube housing assembly, a beam-limiting device, and the necessary supporting structures. Additional components that function with the system are considered integral parts of the system.
Subp. 224.
X-ray tube or tube.
"X-ray tube" or "tube" means an electron tube designed to be used primarily for the production of x-rays.
Statutory Authority:
MS s 144.12
History:
32 SR 777; L 2016 c 119 s 7
Published Electronically:
October 13, 2021
REGISTRATION REQUIREMENTS
4732.0200 REGISTRATION REQUIREMENTS FOR RADIATION-PRODUCING EQUIPMENT AND OTHER ELECTRONIC DEVICES THAT PRODUCE RADIATION.
Subpart 1.
Applicability.
For any facility, except those specifically exempted under this part or part 4732.0300, the person having administrative control of any ionizing radiation-producing equipment must be responsible for completing the registration form and submitting the applicable fee according to Minnesota Statutes, section 144.121. It is the registrant's obligation to keep the information for registration current. Should a change of control result in a change to the registrant's program, the registrant must notify the commissioner of that change according to this part. Persons with administrative control of the radiation-producing equipment must be responsible for maintaining equipment in compliance with a nationally recognized standard, such as Code of Federal Regulations, title 21, section 1020.30, the manufacturer's specifications, or parts 4732.1100 to 4732.1130.
Subp. 2.
New facility.
For a new facility, an application for registration must be submitted to the commissioner and approved prior to the operation of the equipment. Application for registration must be completed on forms furnished by the commissioner or an acceptable alternative and must be complete and accurate. The application must include the appropriate fee established in Minnesota Statutes, section 144.121, subdivision 1a.
B.
The registrant should notify the commissioner within 30 days of the following changes:
(4)
any change in the facility that might impact radiation exposures such as remodeling involving removal of shielded walls or barriers;
(6)
radiation safety officer or other personnel identified on the registration as having responsibility for radiation safety within the facility.
C.
A person shall not refer in any advertisement, to the fact that the ionizing radiation-producing equipment is registered with the commissioner, and shall not state or imply that the commissioner has approved any activity under such registration.
Subp. 3.
Issuance of notice of registration.
A.
Upon receipt of registration, the commissioner shall issue a notice of registration. Each notice of registration shall expire at the end of the indicated month and year.
B.
The commissioner may incorporate in the registration at the time of issuance or thereafter any additional requirements with respect to the registrant's receipt, possession, use, and transfer of radiation-producing equipment as the commissioner deems appropriate or necessary.
Subp. 4.
Renewal of registration.
A.
Renewal of registration must be submitted according to this subpart. Each registrant must renew following the schedule in subpart 5 as long as the activity requiring registration continues.
B.
The registrant must certify by signature or electronic signature that the information is accurate and complete.
C.
If there has been any additional radiation-producing equipment or other substantial change made after the existing registration or renewal, the registrant must include all pertinent information regarding the addition or change.
Subp. 5.
Staggered schedule for renewal of registration.
Each registration under this chapter must be renewed on or before the first day of the calendar quarter specified in items A to D. The following schedule is based on the registrant's business address within the state:
A.
Beginning January 1, 2008: Hennepin County registrants including the University of Minnesota, Minneapolis campus;
C.
Beginning July 1, 2008: Aitkin, Benton, Carlton, Cass, Chisago, Cook, Crow Wing, Isanti, Itasca, Kanabec, Koochiching, Lake Mille Lacs, Morrison, Pine, St. Louis, Becker, Beltrami, Big Stone, Chippewa, Clay, Clearwater, Douglas, Grant, Hubbard, Kittson, Lac Qui Parle, Lake of the Woods, Mahnomen, Marshall, Norman, Otter Tail, Pennington, Polk, Pope, Red Lake, Roseau, Stearns, Stevens, Swift, Todd, Traverse, Wadena, and Wilkin County registrants, and registrants whose business addresses are outside the state; and
D.
Beginning October 1, 2007: Brown, Carver, Cottonwood, Faribault, Jackson, Kandiyohi, Lincoln, Lyon, Martin, McLeod, Meeker, Murray, Nicollet, Nobles, Pipestone, Redwood, Renville, Rock, Sherburne, Sibley, Watonwan, Wright, Yellow Medicine, Blue Earth, Dodge, Fillmore, Freeborn, Goodhue, Houston, Le Sueur, Mower, Olmsted, Rice, Scott, Steele, Wabasha, Waseca, and Winona County registrants.
Subp. 6.
Renewals affected by change of location.
A registrant whose business address changes from one county to another must renew the registration with the county of relocation according to the schedule in subpart 5. The registrant shall not be assessed penalty fees for not renewing with the county of previous location.
Subp. 7.
Change of ownership.
In addition to the notification required in subpart 1, the registration of the facility is not transferable as part of a change in ownership.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0210 REGISTRATION FEES.
The initial registration application or renewal for registration of radiation-producing equipment required under part 4732.0200 must be accompanied by the fee established in Minnesota Statutes, section 144.121, subdivision 1a. The registration fee is nonrefundable.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0220 GENERAL REQUIREMENTS FOR ALL FACILITIES.
Subpart 1.
Responsibilities of registrant.
The registrant must:
A.
ensure compliance with applicable parts of this chapter and in the operation of the equipment that are consistent with each registrant's area of use;
B.
notify the commissioner within 30 days of any change in the ownership, addition of, or disposition of registered radiation-producing equipment; and
Subp. 2.
Submissions.
A.
Any submission of any information provided to the commissioner by a registrant must be complete and accurate in all material submitted.
B.
All communications and reports concerning these regulations, applications, and violations filed thereunder, must be addressed to or delivered to the Minnesota Department of Health, Radiation Control Unit, 625 Robert Street North, P. O. Box 64975, St. Paul, Minnesota 55164-0975.
Subp. 3.
Shielding requirements.
All registrants must maintain documentation of the radiation shielding installed in their facility. The documentation must be:
B.
a shielding plan that was completed by a service provider or an appropriate radiological physicist;
D.
verified by a detailed radiation survey covering radiation levels at the operator position and at pertinent points outside the room during normal operation; and
E.
if the registrant cannot verify shielding compliance by items A to C, a detailed radiation survey covering the radiation levels at the operator position and at pertinent points outside the room during normal operation must be completed and the documentation maintained.
Subp. 4.
Exemption.
Dental facilities with only intraoral capabilities are exempted from the shielding requirements in subpart 3.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0250 RECIPROCITY FOR OUT-OF-STATE RADIATION-PRODUCING EQUIPMENT.
Subpart 1.
Applicability.
Whenever radiation-producing equipment is to be brought into the state for any temporary use, a written notice must be provided to the commissioner at least three working days before the equipment is to be used in the state. Upon request to the department, permission to process use of equipment sooner may be granted if the three-day notification period would impose an undue hardship on the person. The notice required in this subpart must include:
Subp. 3.
Inspections.
Inspections by the commissioner may be performed on any radiation-producing equipment being used in Minnesota on a reciprocal basis for compliance with this chapter.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0275 REGISTRATION OF SERVICE PROVIDERS.
Subpart 1.
Application for service provider registration.
A.
A person who is engaged in the business of assembling, installing, repairing, or replacing one or more components in a radiation-producing equipment system or conducting equipment performance evaluations on diagnostic or industrial radiation-producing equipment must apply for registration with the commissioner within 30 days following the effective date of this chapter or prior to furnishing or offering to furnish any services. The services may include, but are not limited to:
(1)
installing, replacing, or repairing radiation-producing equipment and associated components; and
(2)
performing equipment performance evaluations on diagnostic or industrial radiation-producing equipment and associated components.
B.
All applications for registration must be completed on forms furnished by the commissioner and must include all information specified by the commissioner.
C.
A person applying for registration under this part must specify:
(2)
the training and experience that qualify them to discharge the services for which they are applying for registration;
(3)
the type of measurement instruments to be used, frequency of calibration, and calibration facility; and
Subp. 2.
Issuance of notice of registration.
A.
Upon a determination that an applicant meets the requirements of this chapter, the commissioner shall issue a notice of registration. Each notice of registration expires at the end of the specified day in the month and year stated in the notice.
B.
The commissioner may incorporate in the notice of registration at the time of issuance or after by appropriate rule, or regulation, any additional requirements and conditions deemed appropriate or necessary by the commissioner.
Subp. 3.
Renewal of registration.
Renewal of the registration for service providers must be completed 30 days prior to the end of the month of the current registration.
Subp. 4.
Exemption.
An individual employed by a registrant to perform in-house calibrations, equipment performance evaluations, or repairs of diagnostic or industrial radiation-producing equipment is exempt from registering as a service provider. An in-house employee may not perform these tasks elsewhere unless registered as a service provider.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0280 SERVICE PROVIDER'S RESPONSIBILITY.
Subpart 1.
General requirements.
A person shall not make, sell, lease, transfer, lend, repair, or install radiation-producing equipment or the parts used in connection with this equipment unless the parts and equipment, when properly placed in operation, meet the federal requirements for the equipment manufacturer's specifications and the requirements of this chapter.
Subp. 2.
Notification requirements.
A registered service provider must meet the notification requirements in this subpart.
A.
A person selling, leasing, or transferring radiation-producing equipment must notify the commissioner in writing within 15 days of the sale, lease, or transfer, and must supply the name and address of the purchaser and other pertinent information required by the commissioner.
B.
Installation calibrations and equipment performance test reports must be sent to the facility within 30 days of the tests. The service provider must keep copies of these test reports for four years after completion.
C.
The test reports must include written recommendations for necessary corrections or improvements.
Subp. 3.
Calibration reports at time of installation.
At the time of installation, calibrations must be performed on diagnostic or industrial radiation-producing equipment prior to first use on patients according to nationally recognized standards, such as:
D.
the service provider's written report, which must include:
(4)
the numerical results of the tests including any appropriate films. If the result of the test is not a numerical answer, a pass or fail or "yes" or "no" answer is acceptable;
(5)
any written recommendations necessary for corrective actions to maintain compliance with this chapter; and
Subp. 4.
Equipment performance tests.
At the time of the equipment performance tests, the tests must be completed at intervals not to exceed 24 months. The tests must be performed over the clinical range on the equipment according to parts 4732.1100 to 4732.1130; Code of Federal Regulations, title 21, section 1020; or the manufacturer's specifications. The registered service provider must keep copies of these test reports for four years after completion. The service provider's written report to the facility must include:
D.
the numerical results of the tests including any appropriate films. If the result of the test is not a numerical answer, a pass or fail or "yes" or "no" answer is acceptable;
E.
any written recommendations necessary for corrective actions to maintain compliance with this chapter; and
Subp. 5.
Individual monitoring.
The vendor employing registered service providers must provide individual monitoring devices and reports for their occupational exposure according to part 4732.0440, where applicable.
Subp. 6.
Phantom use.
The use of humans is prohibited for maintenance, demonstration, and training. A phantom must be used for these purposes.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
GENERAL ADMINISTRATION
4732.0300 EXEMPTIONS.
This chapter shall not apply to:
B.
domestic television receivers, provided the dose rate at five cm from any outer surface of ten cm2 is less than 0.5 mrem per hour; and
C.
radiation sources specifically designated by the commissioner as exempt by virtue of being known to be without hazard to health.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0305 PROHIBITED USES.
Subpart 1.
General provision.
An individual shall not be exposed to the useful beam of radiation except for healing arts purposes and only if the exposure has been authorized by a licensed practitioner of the healing arts. Exposure of an individual for the purposes in items A, B, and C is prohibited.
A.
Exposure for training, instruction, demonstration, or research is prohibited except when the research has been approved by an institutional review board and is conducted under federal regulations for the protection of human subjects in research under Code of Federal Regulations, title 21, part 56, or title 45, part 46. Any other exposure of a human subject for the purpose of research may be made only with an approved variance as described in parts 4717.7000 to 4717.7050.
Subp. 2.
Other prohibited radiation dose levels.
A worker shall not be subjected to an occupational radiation dose or a radiation dose for training that would exceed the doses specified in parts 4732.0400 to 4732.0430.
Subp. 3.
Prohibited radiation-producing equipment and procedures.
The following equipment or procedures are prohibited:
D.
the use of direct exposure x-ray film, without intensifying screens, for all radiological imaging other than intraoral dental radiography, therapeutic portal imaging, industrial radiography, and radiographic absorptiometry using readipack film especially designed for radiographic absorptiometry;
G.
the use of mammographic imaging systems not specifically designed by the manufacturer for imaging of the breast.
Subp. 4.
Unauthorized exposure of individual monitoring devices.
Exposure of individual monitoring devices to deceptively indicate a dose delivered to an individual is prohibited.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0306 UNAUTHORIZED USES.
Except as authorized by part 4732.0308, the following equipment or procedures are unauthorized:
A.
hand-held diagnostic imaging devices except forensic examinations during emergency situations provided that all manufacturer's radiation shielding devices are in place;
B.
except for radiation therapy simulators, the use of fluoroscopy by x-ray machine operators for positioning a patient for radiographic imaging, except when done by a licensed practitioner of the healing arts;
C.
the use of fluoroscopy by a person other than a licensed practitioner of the healing arts, physician assistant, registered radiologist assistant, or radiology practitioner assistant when the licensed practitioner of the healing arts, physician assistant, or registered radiologist assistant or radiology practitioner assistant is not physically present in the room, except for maintenance or quality assurance activities, training courses, and animal research procedures being performed by trained individuals;
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0308 VARIANCE IONIZING RADIATION RULES.
Except for parts 4732.0200 and 4732.0210, the commissioner shall, according to the procedures and criteria in parts 4717.7000 to 4717.7050, grant a variance from the requirements of this chapter, if it is determined to be authorized by law, would not endanger life or property, and is otherwise in the public interest.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0310 DATA PRIVACY.
Collection, security, and dissemination of information gathered for registration is governed by Minnesota Statutes, chapter 13.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0315 DELIBERATE MISCONDUCT.
For purposes of this chapter, deliberate misconduct would be a registrant, employee of a registrant, or service provider who knowingly:
A.
engages in deliberate misconduct that causes or would have caused, if not detected, a registrant to be in violation of the rule issued by the commissioner; or
B.
deliberately submits to the commissioner or the registrant information that the person submitting the information knows to be incomplete or inaccurate in some respect.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0320 EMPLOYEE PROTECTION.
Employee protection and employment discrimination issues are governed by Minnesota Statutes, sections 181.931 to 181.935.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0330 RECORDS.
Subpart 1.
Applicability.
A facility required to register with the commissioner must maintain records according to this chapter. If there is a conflict between this chapter and other required retention periods for the same type of record, the longest retention period specified takes precedence.
A.
Each registrant must maintain records showing the receipt, transfer, and disposal of all radiation-producing equipment.
B.
Records of individual monitoring, radiation monitoring, radiation surveys, calibrations, and equipment performance measurements for radiation-producing equipment must be kept according to this part.
D.
At all times, the registrant is responsible for record retention required by this chapter. If the registrant ceases operation for any reason, provisions must be made for record retention required by this chapter.
Subp. 2.
Format and safeguarding records.
A.
A record required under this chapter must be legible throughout the specified retention period. The record can be:
Subp. 3.
Reporting units.
As appropriate, a registrant must use the units of rad, roentgen, or rem or the international systems of units (SI), including the multiples and subdivisions. The registrant must clearly indicate the units on all records required by this chapter.
Subp. 4.
Retention schedule for records.
The registrant must ensure that, when applicable, the records are retained in the facility until the inspection by the commissioner. The following records specified in this subpart must be maintained:
A.
quality control test result records that include documentation of:
(1)
the evaluation of the processor quality control tests; except that current processing quality control films need to be kept for 60 current days;
(3)
the evaluation and associated films of the integrity tests of the personal protective garments;
(5)
equipment performance evaluations complete with all numerical values and films as appropriate;
L.
current copies of the physician assistant's physician-physician assistant agreement recognized by the Minnesota Board of Medical Practice, or the written agreement with the supervising physician for either the registered radiologic assistant or radiologic practitioner assistant.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0335 INSPECTIONS AND TESTING.
Subpart 1.
Inspections.
At all reasonable times during the hours of operation, each registrant must allow the commissioner or commissioner's designee access to the facilities and premises where the radiation-producing equipment is used or stored to inspect and test the radiation-producing equipment. Access also includes inspection of all records under the registrant's control that are required to be kept according to part 4732.0330.
Subp. 2.
Tests.
Each registrant must perform or cause to be performed reasonable procedures that are necessary to ensure radiation safety including, but not limited to tests of:
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0340 VIOLATIONS AND ENFORCEMENT REQUIREMENTS.
Subpart 1.
Notice of violation.
The commissioner must issue a written notice of violation to the regulated facility listing the violations identified during an inspection, incident, or medical event. The notice of violation must require that the regulated facility submit, within 30 days of the date of receipt of the notice or other specified time, a written explanation or statement in reply including:
A.
the corrective steps that have been taken by the registrant and the results achieved through verification tests; or
B.
a plan to correct the identified deficiencies and the date when full compliance will be achieved, if it cannot be achieved within the 30 days; and
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
SHIELDING REQUIREMENTS
4732.0355 GENERAL REQUIREMENTS FOR SHIELDING AGAINST IONIZING RADIATION.
Subpart 1.
Applicability.
This part applies to all regulated facilities constructed or structurally remodeled 90 days after November 5, 2007.
Subp. 2.
Requirements.
The registrant must ensure that the applicable structural shielding requirements specified in parts 4732.0355 to 4732.0380 are met. Structural shielding modifications must be made if an analysis of operating conditions indicates the possibility of an individual receiving an occupational dose or a dose to the public in excess of the limits in parts 4732.0400 to 4732.0430.
Subp. 3.
Shielding details.
The shielding must be constructed so that the protection is not impaired by objects passing through the barriers or embedded in the barriers. The primary and secondary barriers must meet the dose limits in parts 4732.0400 to 4732.0430. This includes, but is not limited to, areas of walls containing wall-mounted image receptors.
Subp. 4.
Operator's booth design requirements.
The operator's booth, exposure control, and viewing system must meet the following specifications:
A.
must have no less than 7.5 square feet (0.7 square meters) of unobstructed floor space with no dimension less than two feet (0.6 meters);
B.
must be located and constructed so the unattenuated direct scattered radiation does not reach the operator in the booth;
D.
the radiation exposure control placement must:
(3)
be placed to allow the operator to use the viewing window or other viewing device from within the booth; and
E.
the viewing system must be designed so that:
(1)
each booth has at least one viewing device that will be placed so that the operator at the control panel may directly observe the patient, any other individual in the room, and any doorway into the room; and
(2)
if the viewing system is a window, the window must satisfy the following additional requirements:
(a)
it must have the same lead equivalency as required in the booth's wall in which it is mounted;
(b)
it must have a minimum viewing area of 350 square inches and must be constructed to afford x-ray operators an unobstructed view of the patient and all entrances into the room; and
(c)
it must be designed so the operator's expected viewing position is at least 18 inches (0.46 meters) from the edge of the booth.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
October 3, 2013
4732.0360 SHIELDING PLAN.
Subpart 1.
Shielding plan applicability.
inety days after November 5, 2007, the registrant is required to have a shielding plan complete for new constructions or structural remodeling of their radiation-producing equipment areas.
Subp. 2.
Shielding plan requirements.
The shielding plan must show all basic assumptions used in the development of the shielding specifications and show, at a minimum:
B.
the normal location of the radiation-producing system's x-ray tube's general direction of the useful beam and the tube's travel and transverse limits;
E.
the structural composition and thickness or lead equivalent of all walls, doors, partitions, and, if occupied spaces above or below, the floor and ceiling of the rooms concerned;
Subp. 3.
Modifications.
The review of shielding plans must not preclude the requirement of additional modifications should a subsequent analysis of operating conditions indicate the possibility of an individual receiving a dose in excess of the dose limits prescribed in parts 4732.0400 to 4732.0430.
Subp. 4.
Shielding review.
Ninety days after November 5, 2007, the shielding plan must be submitted to the commissioner prior to any new construction or structural remodeling.
Subp. 5.
Exemptions.
Exemptions from the shielding review:
E.
if the replacement of a piece of radiation-producing equipment does not increase the risk of radiation beyond the dose limits in parts 4732.0400 to 4732.0430;
F.
self-shielded x-ray systems, such as cabinet x-ray units, x-ray diffraction or fluorescence units with interlocked shield barriers; and
G.
for a self-shielded accelerator, the applicant need not submit an evaluation of a shielding plan if an evaluation by an appropriate regulatory authority has been performed. The applicant must reference the evaluation and maintain a copy of the evaluated shielding plan for commissioner review.
Subp. 6.
Records.
The following shielding plan documentation must be maintained on a permanent basis by the registrant of the facility:
B.
construction, or as-built, documents showing location and amounts of shielding material installed;
E.
all reevaluations of the room shielding relative to changes in utilization that have been made; and
F.
the shielding plan information must include the name of the individual completing the plan and the date on which it was completed.
Subp. 7.
Permanent placard.
A permanent placard must be mounted in the room specifying the amount and type of shielding in all walls, doors, partitions, and, if occupied, spaces above or below the floor and ceiling. If mounting the information is not practical, a registrant may post a notice in the room that describes the document and states where it may be examined.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0365 ADDITIONAL SHIELDING REQUIREMENTS FOR DENTAL FACILITIES.
In addition to parts 4732.0355 and 4732.0360 the following shielding requirements are required.
A.
When radiographic systems are installed in adjacent rooms or areas, protective barriers must be provided between the rooms or areas to ensure that the doses are as low as reasonably achievable (ALARA) and do not exceed the dose limits in parts 4732.0400 to 4732.0430.
B.
Each installation must be provided with a protective barrier for the operator or must be arranged so the operator can stand at least six feet from the patient and the tube head and not be in the path of the useful beam.
C.
Protective barriers must be arranged so that the operator is able to view the patient and all entrances to the area during the exposure.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0370 ADDITIONAL SHIELDING REQUIREMENTS FOR INDUSTRIAL FACILITIES USING RADIATION-PRODUCING EQUIPMENT.
Subpart 1.
Industrial facilities.
Industrial facilities must meet the applicable requirements of parts 4732.0355 and 4732.0360 and the shielding requirements in subparts 2 to 4.
Subp. 2.
Applicability.
This part applies to all new construction and structural remodeling that commences 90 days after November 5, 2007.
Subp. 3.
General shielding and design requirements for industrial radiography.
Facilities must be designed to ensure that the dose limits in parts 4732.0400 to 4732.0430 are not exceeded. Stationary industrial ionizing radiation-producing facilities must have fixed protective barriers, except for entrance doors or beam interceptors. The control panel must be located outside the radiography room.
Subp. 4.
Exception.
Registrants who possess cabinet x-ray systems, industrial cabinet baggage x-ray systems, portable industrial x-ray systems, and analytical ionizing radiation-producing equipment are exempt from this part.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0380 SHIELDING REQUIREMENTS FOR ACCELERATORS.
Subpart 1.
Applicability.
This part applies to accelerators and is in addition to other applicable parts of this chapter.
Subp. 2.
Design requirements for accelerator facilities.
Accelerator facilities must have the following safety features:
A.
be designed with primary and secondary barriers to ensure compliance with the dose limits in parts 4732.0400 to 4732.0430;
D.
accelerator room entrances must be provided with warning lights in readily observable positions near the outside of all access doors to indicate when the useful beam is in the "on" position;
E.
interlocks or safety devices must be in place so all access into the room is blocked before irradiation is initiated or continued. If the useful radiation beam is interrupted by any door opening or tripping of the safety device, it must not be possible to restore the system to operation without closing the door or resetting the safety device and reinitiating irradiation by manual action at the control panel;
F.
an emergency power cutoff switch must be located on either side of the primary beam and easily identifiable in all high radiation areas. The cutoff switch must include a manual reset so that the accelerator cannot be restarted from the accelerator control console without resetting the cutoff switch;
G.
instrumentation, readouts, and controls on the accelerator control console must be clearly identified, easily discernible, and located outside the high radiation area;
H.
each entrance into a target area or other high radiation area must be provided with two safety interlocks that shut down the machine when the barrier is breached;
I.
each safety interlock must be on a circuit that allows it to operate independently of the accelerator; and
J.
all safety interlocks must be designed so that any defect or component failure in the safety interlock system prevents operation of the accelerator.
Subp. 3.
Additional design requirements for medical use accelerators.
A.
Closed-circuit television, or an equivalent system, must be provided to permit continuous observation of the patient during irradiation and must be located so the operator may observe the patient from the control panel.
B.
Two-way audio communication between the patient and the operator must be provided at the control panel. However, where excessive noise levels or treatment requirements make audio communication impractical, other methods of communication must be used.
Subp. 4.
Modification of an accelerator or room before use.
If radiation surveys indicate that an individual in an unrestricted area may be exposed to levels of radiation greater than those permitted by part 4732.0430 before use, the registrant must:
A.
equip the unit with beam direction interlocks or add additional radiation shielding to ensure compliance with part 4732.0430;
C.
include the initial radiation survey, a description of the modification made, and the results of the subsequent survey; or
Subp. 5.
Radiation surveys.
A.
The registrant must ensure that radiation surveys are performed at intervals not to exceed 12 months. The radiation survey must be performed with the accelerator in a "BEAM-ON" condition, with the largest available field and with a scattering phantom in the useful beam of radiation, if applicable, to ensure that radiation levels in restricted areas are not likely to cause personnel exposures in excess of the limits specified in parts 4732.0400 to 4732.0430. A radiation survey must also be performed:
(4)
before using the accelerator in a manner that could result in increased radiation levels in areas outside shielded area.
B.
The radiation survey record must also include:
(5)
the measured dose rate at several points in each area expressed in millirems or microsieverts per hour;
(6)
the calculated maximum level of radiation over a period of one year for each restricted and unrestricted area; and
(7)
the signature or electronic signature of the individual responsible for conducting the survey.
Subp. 6.
Corrective actions.
If the results of the radiation surveys indicate any radiation levels in excess of the limits in parts 4732.0400 to 4732.0430 the registrant must lock the control in the "OFF" position and not use the unit except as follows:
B.
until the registrant has submitted a corrective action plan and received authorization in writing from the commissioner.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0385 CAUTION SIGNS.
Subpart 1.
Standard radiation symbol and labeling.
Each radiation sign or label must bear the standard symbol specified in this subpart and the printed warning, in capital block letters, specified in subpart 4. The standard symbol for designating any radiation hazard is a circle with three propeller-like blades arranged around it as illustrated:
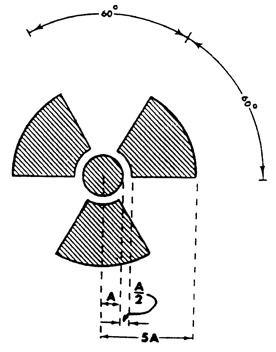
Subp. 2.
Additional information on signs and labels.
In addition to the contents of signs and labels prescribed in this part, the registrant must provide, on or near the required signs and labels additional information, as appropriate, to make individuals aware of potential radiation exposures and to minimize the exposures.
Subp. 3.
Prohibitions on use of symbol.
The use of the specified radiation symbol for any purpose other than designating or referring to an area of applicable radiation levels is prohibited.
Subp. 4.
Posting and labeling requirements.
Conspicuous radiation warning labels must be posted in areas in which a radiation hazard may exist.
A.
The warning "CAUTION RADIATION AREA" or "DANGER RADIATION AREA" must appear on signs in an area in which a radiation hazard may exist.
B.
The warning "CAUTION HIGH RADIATION AREA" or "DANGER HIGH RADIATION AREA" must appear on signs in an area in which a high radiation hazard may exist.
C.
The warning "CAUTION VERY HIGH RADIATION AREA" or "DANGER VERY HIGH RADIATION AREA" must appear on signs in an area in which a very high radiation hazard may exist.
D.
Analytical ionizing radiation-producing equipment complying with part 4732.1000 must be labeled with a readily discernible sign or signs bearing the radiation symbol and the words:
(1)
"CAUTION - HIGH INTENSITY X-RAY BEAM," or words having a similar intent, on the radiation-producing equipment housing; or
(2)
"CAUTION RADIATION - THIS EQUIPMENT PRODUCES IONIZING RADIATION WHEN ENERGIZED," or words having a similar intent, by any switch that energizes an x-ray tube.
Subp. 5.
Exceptions to posting requirements.
A.
A registrant is not required to post caution signs because of the presence of radiation machines used solely for diagnosis in the healing arts.
B.
Rooms in hospitals or clinics that are used for teletherapy are exempt from the requirement to post caution signs under this part if:
(2)
personnel in attendance take necessary precautions to prevent the inadvertent exposure of workers, other patients, and members of the public to radiation in excess of the limits established in this chapter.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
April 25, 2023
DOSE LEVELS
4732.0400 DETERMINATION OF ACCUMULATED OCCUPATIONAL DOSE.
Subpart 1.
Determination of prior occupational dose.
For each individual who is likely to receive in a year, an occupational dose requiring monitoring according to part 4732.0440, the registrant must:
Subp. 2.
Complying with determination of prior occupational dose.
A.
A registrant may:
(1)
accept, as a record of the occupational dose that the individual received during the current year, a written signed statement from the individual or from the individual's most recent employer for work involving radiation exposure that discloses the nature and amount of any occupational dose that the individual received; or
(2)
accept as the record of cumulative radiation dose, an up-to-date form, signed by the individual and countersigned by an appropriate official of the most recent employer for work involving radiation exposure, or the individual's current employer, if the individual is not employed by the registrant.
C.
If the registrant is unable to obtain a complete record of an individual's current and previously accumulated occupational dose, the registrant must assume:
(1)
the allowable dose limits for the individual is reduced by 1.25 rem (12.5 mSv) for each quarter for which records were unavailable and the individual was engaged in activities that could have resulted in occupational radiation exposure; and
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0410 OCCUPATIONAL DOSE LIMITS FOR ADULTS.
Subp. 2.
Occupational dose control.
The registrant must control the occupational dose to individual adults, except for planned special exposures, according to part 4732.0425, to the following annual dose limit, which is the more limiting of:
B.
the sum of the deep dose equivalent and the committed dose equivalent to any individual organ or tissue other than the lens of the eye being equal to 50 rem (0.5 Sv); and
Subp. 3.
Doses in excess of limits.
Doses received in excess of the annual limits, including doses received during accidents, emergencies, and planned special exposures, must be subtracted from the limits for planned special exposures that the individual may receive during the current year.
Subp. 4.
Dose equivalent.
A.
The assigned deep dose equivalent and shallow dose equivalent must be for the portion of the body receiving the highest exposure.
B.
The deep dose equivalent, lens dose equivalent, and shallow dose equivalent may be assessed from surveys or other radiation measurements for the purpose of demonstrating compliance with the occupational dose limits if the individual monitoring device was not in the region of highest potential exposure or the results of individual monitoring are unavailable.
C.
When a protective apron is worn while working with fluoroscopic equipment and monitoring is conducted as specified in part 4732.0440, subpart 3, the effective dose equivalent for external radiation must be determined as follows:
(1)
when only one individual monitoring device is used and it is located at the neck (collar) outside the protective apron, the reported deep dose equivalent must be the effective dose equivalent for external radiation; or
(2)
when only one individual monitoring device is used and it is located at the neck (collar) outside the protective apron, the reported deep dose equivalent value multiplied by 0.3 must be the effective dose equivalent for external radiation; or
(3)
when individual monitoring devices are worn, both under the protective apron at the waist and outside the protective apron at the neck, the effective dose equivalent for external radiation must be assigned the value of the sum of the deep dose equivalent reported for the individual monitoring device located at the waist under the protective apron multiplied by 1.5 and the deep dose equivalent reported for the individual monitoring device located at the neck outside the protective apron multiplied by 0.04.
Subp. 5.
Reduction of dose.
The registrant must reduce the dose that an individual may be allowed to receive in the current year by the amount of occupational dose received while employed by any other person during the current year.
Subp. 6.
Dose information.
The employee must supply information to the registrant about other current occupational doses received due to employment at multiple facilities.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0415 DOSE EQUIVALENT TO AN EMBRYO OR FETUS.
A.
When a woman declares her pregnancy in writing, the registrant must ensure that the dose equivalent to an embryo or fetus during the entire pregnancy, due to occupational exposure of a declared pregnant woman, does not exceed 0.5 rem (5 mSv). Records must be kept according to part 4732.0440.
B.
The registrant must make efforts to avoid substantial variation above a uniform monthly exposure rate to a declared pregnant woman to satisfy the limit in item A.
C.
A registrant must make a reasonable effort to limit the occupational dose to the embryo or fetus to 0.05 rem (0.5 mSv) in any one month of pregnancy, excluding medical exposure.
D.
If the dose to the embryo or fetus is found to have exceeded 0.5 rem (5 mSv) or is within 0.05 rem (0.5 mSv) of this dose by the time the woman declares her pregnancy, the registrant must ensure that additional occupational dose equivalent to the embryo or fetus does not exceed 0.05 rem (0.5 mSv) during the remainder of the pregnancy.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0420 EXPOSURE OF MINORS.
A registrant shall not use sources of radiation in a manner that causes an individual within a restricted area who is under 18 years of age to receive an occupational radiation dose greater than ten percent of the annual occupational dose limits specified for adult workers in part 4732.0410.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0425 PLANNED SPECIAL EXPOSURES.
A registrant may authorize an adult worker to receive doses in addition to and accounted for separately from the doses received under the limits in part 4732.0410, subpart 2, provided that each of the following conditions is satisfied:
A.
the registrant authorized a planned special exposure only in an exceptional situation when alternatives that might avoid the dose estimated to result from the planned special exposure are unavailable or impractical;
B.
the registrant and employer, if the employer is not the registrant, specifically authorizes the planned special exposure, in writing, before the exposure occurs;
C.
before a planned special exposure, the registrant ensures that each individual involved is:
(2)
informed of the estimated doses and associated potential risks and specific radiation levels or other conditions that might be involved in performing the task;
(3)
instructed in the measures to be taken to keep the dose ALARA considering other risks that may be present; and
D.
prior to permitting an individual to participate in a planned special exposure, the registrant ascertains prior doses as required by part 4732.0400 during the individual's lifetime;
E.
subject to part 4732.0410, the registrant must not authorize a planned special exposure that would cause an individual to receive a dose from all planned special exposures and all doses in excess of the limits to exceed:
F.
the registrant records the best estimate of the dose resulting from the planned special exposure in the individual's record and informs the individual, in writing, of the dose within 30 days from the date of the planned special exposure. The dose from planned special exposures must not be considered in controlling future occupational dose of the individual according to part 4732.0610, subpart 2, but must be included in dose determinations required by part 4732.0410.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0430 DOSE LIMITS FOR INDIVIDUAL MEMBERS OF THE PUBLIC.
A.
A registrant shall not use radiation-producing equipment in a manner that could result in individual members of the public receiving an annual effective dose equivalent in excess of 0.1 rem (1.0 mSv).
B.
The registrant must conduct operations so that the dose in any unrestricted area does not exceed 0.002 rem (0.02 mSv) in any one hour.
C.
The registrant must show compliance with the annual public dose limit in this part, by demonstrating by measurement or calculation that the total effective dose equivalent to the individual member of the public likely to receive the highest dose from the registered operation does not exceed the annual dose limit.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0440 INDIVIDUAL MONITORING.
Subpart 1.
Applicability.
Each registrant must supply the following personnel with appropriate individual monitoring devices and require the personnel to wear the monitoring devices:
A.
adults likely to receive in one year, a dose in excess of ten percent of the limits in part 4732.0410;
B.
declared pregnant women likely to receive, during the entire pregnancy, a dose in excess of 0.1 rem (1.0 mSv);
Subp. 2.
Assignment.
Each individual monitoring device must be assigned to and worn by only one individual.
Subp. 3.
Placement of individual monitoring device.
Each registrant must ensure that individuals who are required to be monitored for occupational doses according to this part wear individual monitoring devices as follows:
A.
an individual monitoring device used for monitoring the dose to the whole body must be worn on the trunk of the body or at the unshielded location of the whole body likely to receive the highest exposure;
B.
when a protective apron is worn, the individual monitoring device must be worn at the collar outside of the protective apron;
C.
when more than one individual monitoring device is used, the record must identify the location of the monitor on the body and must state whether it was worn outside or under the protective clothing. The effective dose equivalent must be recorded in the reports required by this part; and
Subp. 4.
Individual monitoring control devices.
The registrant must obtain a control device that accompanies individual personal monitoring devices during shipment. The control device must be kept in an area of natural background radiation at the facility between shipments.
Subp. 5.
Veterinary facilities.
Veterinary facility requirements for individual monitoring have been repealed from Minnesota Statutes, section 144.121, subdivision 4. Veterinary staff must follow occupational dose limits for individual monitoring in this part.
Subp. 6.
Industrial facilities.
The registrant in an industrial radiography facility must not permit an individual to act as a radiographer or a radiographer's assistant unless the individual wears a combination of a direct reading dosimeter, an alarming ratemeter, and an individual monitoring device at all times during radiographic operations. The use of electronic dosimeters must only be used in place of ion-chamber pocket dosimeters.
Subp. 7.
Exception for permanent industrial radiographic installations.
At permanent industrial radiographic installations where other appropriate alarming or warning devices are in use, an alarming ratemeter and a direct reading dosimeter are not required.
Subp. 8.
Exception for industrial pulsed x-ray devices.
Alarming ratemeters are not required for individuals using industrial pulsed x-ray devices.
Subp. 9.
Direct reading pocket dosimeters.
When direct reading pocket dosimeters are used, the registrant must:
C.
check the pocket dosimeters at intervals not to exceed 12 months for correct response to radiation. Acceptable dosimeters must read within plus or minus 20 percent of the true radiation exposure; and
Subp. 10.
Off-scale dosimeters.
If an individual's monitoring device is found to be off-scale or the electronic personal dosimeter reads greater than 200 mrem (2 mSv):
B.
the individual may not resume work associated with the use of radiation-producing equipment until a determination of the individual's radiation exposure has been made by the radiation safety officer or the radiation safety officer's designee; and
Subp. 11.
Lost or damaged direct reading pocket dosimeters.
If an individual monitoring device is lost or damaged the registrant must require the worker to cease work immediately until a replacement is provided and the dose is calculated for the time period from issuance to loss or damage.
Subp. 12.
Alarming ratemeters.
To ensure correct response to radiation, each alarming ratemeter must:
B.
be set to sound at a preset exposure rate less than or equal to 500 mR/hr (1.29 x 10-4 C/kg/hr), except for industrial radiography where it must be set at 500 mR/hr (1.29 x 10-4 C/kg/hr);
E.
sound, vibrate, activate a light, or otherwise signal within plus or minus 20 percent of the true radiation exposure rate.
Subp. 13.
Individual monitoring dosimetry records.
A.
A registrant must maintain records showing the radiation doses of all individuals for whom individual monitoring is required according to this part. The records must be clear and legible.
B.
The registrant must retain records of individual doses for the lifetime of the individual worker or a minimum of 30 years after termination of employment with the facility, whichever is less.
Subp. 14.
Individual monitoring reports.
A.
A registrant must advise each worker annually of the worker's dose of radiation as shown in records maintained by the registrant according to this part.
C.
At the request of a worker formerly engaged in registered activities controlled by the registrant, the registrant must furnish to the worker a written report of the worker's exposure to radiation as shown in records maintained by the registrant according to part 4732.0330. The report required by this item must:
(2)
within 30 days after the registrant has determined the dose of the individual, whichever is later.
D.
A registrant must furnish a report of the worker's dose of radiation to a worker who is terminating employment, or to a worker who while employed by another person is terminating a work assignment involving radiation dose in the registrant's facility. This report must:
(1)
be provided to the worker within 30 days after the exposure has been determined by the registrant;
(2)
cover each calendar quarter in which the worker's activities involved exposure to radiation; and
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
RADIATION SAFETY REQUIREMENTS
4732.0500 REGISTRANT'S SAFETY RESPONSIBILITIES.
Subpart 1.
Applicability.
The registrant is responsible for the operation of radiation-producing equipment under the registrant's administrative control and must ensure that the requirements of this chapter are met.
Subp. 2.
Designation of radiation safety officer.
A.
If the registrant is not the radiation safety officer, the registrant must appoint a radiation safety officer. The individual must be qualified by training and knowledge concerning radiation hazards and precautions involved in the operation of the radiation-producing equipment.
B.
The individual designated as a radiation safety officer must be either a licensed practitioner of the healing arts; or an individual who has completed training in the following items:
C.
The radiation safety officer must agree in writing to be responsible for implementing the radiation protection program.
D.
The registrant, through the radiation safety officer, must ensure that radiation safety activities are being performed according to registrant-approved procedures and this chapter.
E.
The registrant must provide the radiation safety officer sufficient authority, organizational freedom, time, resources, and management prerogative to:
Subp. 3.
Individuals who may apply radiation to humans.
Only those individuals who are licensed practitioners of the healing arts, physician assistants, registered radiologic assistants or radiology practitioner assistants, or individuals who have successfully passed an examination under Minnesota Statutes, section 144.121, subdivision 5, may apply radiation to an individual.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0505 RADIATION SAFETY OFFICER RESPONSIBILITIES.
The individual who is the radiation safety officer must:
A.
establish a quality assurance program for compliance with the applicable requirements of this chapter;
B.
review the quality assurance program content and implementation at intervals not to exceed 12 months;
C.
ensure that instructions concerning hazards and safety practices are provided to individuals under the radiation safety officer's supervision who may be exposed to radiation;
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0510 PROCEDURES AND SAFETY INSTRUCTION FOR FACILITIES.
Subpart 1.
Training requirement.
An individual operating radiation-producing equipment must be instructed initially in facility specific and system specific safe operating procedures, emergency procedures, quality control procedures, and the proper protective shielding to be used. Additional training must be conducted at the time of any change to the quality assurance program or change in radiation output.
Subp. 2.
Safety procedures for the facility.
A.
The registrant must maintain safety procedures including patient holding, if applicable, and any restrictions of the operating technique required for the safe operation of the particular system. The procedures must be made available to x-ray operators.
B.
All individuals who, in the course of employment in a year, are likely to receive an occupational dose in excess of 100 millirems (1.0 mSv) must be:
(2)
instructed in the health protection problems associated with exposure to radiation, in precautions to procedures to minimize exposure, and in purposes and functions of protective devices employed;
(3)
instructed of their responsibility to report promptly to the registrant any condition that leads to or causes a violation of this chapter or any unnecessary exposure to radiation; and
(4)
instructed in the appropriate response to warnings made in the event of any malfunction that involves exposure to radiation.
Subp. 3.
Exposure of individuals other than patient.
Except for the patient, only the staff, ancillary personnel, or nonmedical persons required for the medical, dental, and veterinary medical procedures or training must be in the room during the radiographic exposure. All individuals including staff, ancillary personnel, or nonmedical persons required for assistance with the radiographic procedures must be positioned so that no part of the body will be struck by the useful beam unless protected by 0.5 millimeter lead equivalent material.
A.
During any radiographic or fluoroscopic exposure, any door that is part of the protective barrier must be closed.
B.
No individual other than the patient must be in a therapy treatment room during exposures from a therapeutic x-ray system operating above 150 kVp.
Subp. 4.
Gonad protection.
Except for cases in which it would interfere with the diagnostic procedure, during radiographic procedures in which the gonads are in or within two inches (5cm) of the useful beam, gonad shielding of not less than 0.5 millimeters lead equivalence must be used for patients who have procreative potential.
Subp. 5.
Holding.
When a patient, film cassette, or intraoral film must be provided with auxiliary support during a radiation exposure, the following conditions apply:
B.
safety procedures, as required by subpart 2, must indicate the requirements for selecting the individual holding and the procedure that the individual must follow;
C.
the human holder must be instructed in personal radiation safety and protected as required by subpart 2, item B, subitem (2); and
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0520 QUALITY ASSURANCE PROGRAM.
Subpart 1.
General requirements.
A registrant conducting radiographic or therapeutic procedures using radiation-producing equipment must implement a site-specific quality assurance program. The program must include:
C.
the equipment performance tests which are to be completed at intervals not to exceed 24 months and related evaluation documentation, including films, as appropriate, as specified in nationally recognized standards, according to:
(1)
Code of Federal Regulations, title 21, section 1020.30, for diagnostic equipment and Code of Federal Regulations, title 21, section 892, for therapeutic equipment;
D.
the documentation of any correction of any deficiencies found during the equipment performance tests and verification of the actions taken;
E.
when an operating parameter has been exceeded, the radiation-producing equipment must not be used or must be limited to those uses permitted by the registrant, radiation safety officer, or physicist by established written procedures for no longer than 14 days until corrective actions have been taken and verified to have corrected the out-of-limits parameters;
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0530 ALARA PROGRAM.
The registrant must use, to the extent practical, procedures and engineering controls based upon sound radiation protection principles to achieve occupational doses and dose to the public that are as low as is reasonably achievable and do not exceed the dose limits in parts 4732.0410 to 4732.0430.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0535 RETAKE OR REJECT ANALYSIS PROGRAM.
Subpart 1.
Applicability.
Except for dental facilities, for radiographs or images used in patient diagnosis, the registrant will perform or have performed an analysis of the retaken or rejected radiographs or images used in patient diagnosis:
B.
facilities must include the retake or reject analysis results in the audit according to part 4732.0540;
C.
the analysis must include at a minimum, the overall retake or reject rate and a summary of the causes for the retakes or rejects; and
D.
the registrant or radiation safety officer must design the facility specific procedures for the retake and reject analysis. The written procedure must be included in the facility operating procedures.
Subp. 2.
Corrective actions.
Appropriate corrective actions taken based on the results of the analysis must be documented.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0540 RADIATION PROGRAM AUDITS.
Subpart 1.
Applicability.
A registrant must ensure that the quality assurance program, its content, and implementation are reviewed annually. The radiation program audit in this part must be reviewed for compliance with this chapter.
Subp. 2.
Procedures.
The registrant must ensure that all radiation program audits are performed according to procedures established by the registrant or radiation safety officer.
Subp. 3.
Corrective actions.
Any noncompliance issues found during the audit must be corrected and documented. The radiation safety officer must review any corrective actions.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0545 UTILIZATION LOG.
A.
Excluding dental facilities, facilities performing radiographic or fluoroscopic procedures must maintain a utilization log containing:
(6)
the name of the human holder when the patient or film must be provided with human auxiliary support;
(7)
utilization logs for fluoroscopic equipment without a dose-area-product monitor must include the patient's exposure received per fluoroscopic procedure in excess of five minutes; and
(8)
utilization logs for fluoroscopic equipment with a dose-area-product monitor must include the patient's exposure received per fluoroscopic procedure in excess of five minutes.
B.
Facilities performing industrial radiography must maintain a utilization log containing:
(4)
the technique factors specifying the voltage, current, exposure time for each radiographic exposure, and number of exposures; and
C.
Facilities using radiation-producing equipment for gauging must maintain a utilization log containing:
D.
Industrial cabinet, baggage units, and ion implanters are exempt from the requirements of this part.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0550 RADIOLOGICAL PRACTICE STANDARDS.
Subpart 1.
Required standards.
The following procedures and auxiliary equipment designed to minimize patient and personnel exposure must be used.
A.
The speed of screen-film combinations, or direct exposure x-ray film in intraoral dental radiography, must be the fastest speed consistent with the diagnostic objective of the examinations.
B.
Except for dental intraoral films and radiation therapy port films, intensifying screens must be used in combination with the compatible film.
C.
The radiation exposure to the patient must be the minimum exposure required to produce images of good diagnostic quality utilizing the ALARA concept.
D.
Portable x-ray equipment must be used only for examinations where it is impractical to transfer the patient to a stationary x-ray system.
E.
Other than fluoroscopic and dental intraoral systems, radiographic systems must not be used in procedures where the source-to-skin distance is less than 11.8 inches (30 centimeters), except as described in part 4732.0825.
F.
Personal protective garments must be monitored for integrity initially and at intervals not to exceed 24 months.
Subp. 2.
Radiographic technique chart.
A radiographic technique chart must be provided in the vicinity of the x-ray system's control panel.
A.
The technique chart must specify the following information for all examinations:
(4)
for automatic exposure control (AEC) or phototimed units, the percent differences between the AEC increments.
B.
For computed tomography systems, a current technique chart for each routine examination and the computed tomography conditions of operation must be provided.
C.
For filmless radiography, including computed radiography, digital radiography, computed tomography systems, and photostimulable storage phosphor imaging, the technique chart must reflect the adult and pediatric technique parameters for the individual system. This includes the manufacturer's requirements for technique parameters.
Subp. 3.
Exceptions.
Diagnostic radiation-producing equipment manufactured with anatomical programming and industrial facilities with radiation-producing equipment are exempt from subpart 2.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0555 X-RAY FILM PROCESSING REQUIREMENTS.
Subpart 1.
Processing equipment.
A facility with a radiographic x-ray system using radiographic film must have available suitable equipment for handling and processing radiographic film according to the following provisions.
A.
Manual processing:
(1)
the temperature of solutions in the tanks must be maintained within the range of 60 degrees Fahrenheit to 80 degrees Fahrenheit (15.6 degrees Celsius to 16.7 degrees Celsius);
(2)
film must be developed according to the time-temperature relationships recommended by the film and chemistry manufacturers, or in the absence of such recommendations, with the following time-temperature chart:
Time-Temperature Chart
| Thermometer Reading Celsius Degrees |
Thermometer Reading Fahrenheit Degrees |
Minimum Developing Time (Minutes) |
| 26.7 | 80 | 2 |
| 26.1 | 79 | 2 |
| 25.6 | 78 | 2-1/2 |
| 25.0 | 77 | 2-1/2 |
| 24.4 | 76 | 3 |
| 23.9 | 75 | 3 |
| 23.3 | 74 | 3-1/2 |
| 22.8 | 73 | 3-1/2 |
| 22.2 | 72 | 4 |
| 21.7 | 71 | 4 |
| 21.1 | 70 | 4-1/2 |
| 20.6 | 69 | 4-1/2 |
| 20.0 | 68 | 5 |
| 19.4 | 67 | 5-1/2 |
| 18.9 | 66 | 5-1/2 |
| 18.3 | 65 | 6 |
| 17.8 | 64 | 6-1/2 |
| 17.2 | 63 | 7 |
| 16.7 | 62 | 8 |
| 16.1 | 61 | 8-1/2 |
| 15.6 | 60 | 9-1/2 |
(3)
thermometers must be used to indicate the actual temperature of the developer and a timer used to ensure the correct development time.
B.
Automatic processing:
(1)
films must be developed according to the time-temperature relationship recommended by the film and chemistry manufacturer;
(2)
the registrant must have a copy of the film or chemical manufacturer's developing recommendations available for the operators. The developing recommendations must be available for inspection;
(3)
thermometers must be used to verify the actual chemical temperatures to ensure they fall within manufacturer's specifications. If the processing equipment does not have a digital readout or ready light, the temperature must be checked daily, otherwise weekly temperature verification must be completed and documented.
Subp. 2.
Processing quality control.
A.
Processing quality control testing must be performed each day prior to any diagnostic films being processed at the facility. This is to be done by using:
(2)
dental facilities with both extraoral and intraoral equipment using one processing method must use:
(3)
dental facilities with only intraoral equipment must use a dental radiographic normalizing and monitoring device for the processor quality control test especially designed for intraoral processors;
(4)
dental facilities with panoramic equipment with an automatic step wedge program installed by the manufacturer, must use that program for processor quality control;
(5)
dental facilities with both extraoral and intraoral equipment that use two processing methods must use either subitem (2) and item B or subitems (2) and (3) depending on the type of extraoral equipment installed;
(6)
medical or dental facilities that process less than ten patient films in a week may do the processing quality control test on the first day of the week; and
B.
The sensitometry test in item A, subitem (1), must be performed and evaluated using the most sensitive clinical film or mammographic film if mammography films are processed in the same processor as other patient films.
Subp. 3.
Darkroom or glove box fog tests.
A.
The darkroom or glove box must be free of extraneous light and use proper safe lighting so that any film type in use when exposed to x-radiation will not suffer an increase in density during processing. If used, daylight film handling boxes must preclude fogging of the film.
B.
The darkroom or glove box must be tested for film fog using the most sensitive clinical film or mammographic film if mammography films are processed in the same darkroom as other patient films. Tests for the film fog must be completed:
C.
In medical facilities, the amount of fog, the increase in optical density, for a two-minute test must not exceed 0.08 for radiographic film development.
D.
In dental facilities with extraoral equipment, the amount of fog for a two-minute test must not exceed one step on either side of the designated step when using the step wedge for the fog test.
E.
In dental facilities with intraoral equipment only, the amount of fog for a two-minute test must not allow visualization of the outline of a coin on the intraoral film.
Subp. 4.
Outdated x-ray film.
Outdated x-ray film must not be used for diagnostic radiographs, unless the film has been stored according to the manufacturer's recommendations and passes the sensitometric test, step wedge test, or the dental radiographic normalizing and monitoring device test for normal ranges of base plus fog and speed.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0560 ORDERING OF DIAGNOSTIC RADIOGRAPHIC OR THERAPEUTIC PROCEDURES.
Subpart 1.
Applicability.
Except when the radiographic procedure is part of a healing arts screening program approved by the commissioner, the registrant must be responsible for ensuring that the requirements in subpart 2 on ordering radiographic or therapeutic procedures are met.
Subp. 2.
Diagnostic radiographic procedure orders.
A.
The order for a radiographic examination can be made only by a licensed practitioner of the healing arts, a certified clinical nurse specialist, certified nurse midwife, certified nurse practitioner, or physician assistant. The physician assistant must show eligibility to order radiographic procedures through the physician assistant's written physician-physician assistant agreement with a copy on site at the facility.
B.
The operator must not carry out a radiographic procedure unless ordered by individuals listed in this subpart.
C.
An order for a radiographic procedure must be available to procedure personnel at the time of the examination.
D.
The order for a radiographic procedure must include:
(2)
identification of the individual ordering the examination, through either a signature, electronic signature, or equivalent procedure;
E.
A licensed dental hygienist may order radiographs in facilities under a collaborative agreement authorized by the Board of Dentistry under Minnesota Statutes, chapter 150A.
Subp. 3.
Exception for dental facilities.
Dental facilities are exempt from the provisions of subpart 2 for recall patients provided:
Subp. 4.
Therapeutic procedure orders.
A.
The order for radiation therapeutic treatments can be made only by a licensed practitioner of the healing arts or a physician assistant supervised by a therapeutic radiologist or a radiation oncologist. The physician assistant must show eligibility to order therapeutic procedures through a written delegation agreement with a copy on site at the facility.
B.
The operator must not carry out radiation therapeutic treatments unless ordered by individuals listed in this subpart.
C.
An order for radiation therapeutic treatments must be available to personnel at the time of the treatment.
Subp. 5.
Identification prior to administration of treatment.
Prior to each administration of a treatment series, the patient's identity must be verified as the individual named in the procedure order. This should be done using two means of identification.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0565 HEALING ARTS SCREENING.
Subpart 1.
General requirements.
A person proposing to conduct a healing arts screening program must not implement the program without prior approval of the commissioner. An applicant must meet the requirements in this chapter. In addition:
A.
an applicant must be registered with the commissioner before application for screening is initiated; and
B.
the applicant must submit the information in this part on an application form provided by the commissioner or an equivalent form.
Subp. 2.
Content of application.
In the application for screening, the applicant must provide:
B.
each location of the proposed screening and the name and telephone number of a contact person at each location;
C.
the purpose of the proposed screening program planned. This purpose must include the diseases or conditions for which the x-ray examinations are to be used in diagnoses;
E.
a description of the population to be examined in the screening program, for example, age, sex, physical condition, and other appropriate information;
F.
an evaluation of any known alternate methods not involving ionizing radiation that could achieve the goals of the screening program and why these methods are not used instead of the x-ray examinations;
G.
an evaluation by a diagnostic radiological physicist of the x-ray systems to be used in the screening program. The evaluation must show that the system satisfies all requirements of these regulations;
H.
a measurement of patient exposures from the x-ray examination to be performed during the screening;
L.
the qualifications of the individual who will be supervising the operators of the x-ray system. The extent of supervision and the method of work performance evaluation must be specified;
M.
a list of the name(s), business address(es), and qualifications of the individual(s) who will interpret the radiographs;
N.
the procedures for informing the individuals screened and their private practitioners of the healing arts of the results of the screening procedure and any further medical needs indicated;
O.
the procedures for the retention or disposition of the radiographs and other records pertaining to the x-ray examinations;
Subp. 3.
Notification of commissioner's decision.
The applicant must be notified in writing of the commissioner's decision.
Subp. 4.
Changes in screening program.
The applicant is responsible for informing the commissioner of any changes in the screening program described in the application. The applicant must obtain commissioner approval of the changes before the implementation.
Subp. 5.
Appeal procedure.
The applicant may appeal the denial or refusal to approve an application or renewal application by requesting a contested case hearing under the provisions of the Administrative Procedure Act, Minnesota Statutes, chapter 14. The applicant must submit, within 15 days of the receipt of the department's decision, a written request for a hearing. The request for a hearing must set forth in detail the reasons why the applicant contends that the decision of the department should be reversed or modified.
Subp. 6.
Renewal of screening program application.
Any request for the renewal of a screening program application must be submitted in writing 30 days before its expiration date. Renewal requests must contain the information specified in subpart 2.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0570 OPERATOR REQUIREMENTS.
Except for an individual licensed under Minnesota Statutes, chapter 147, 147A, 150A, or 153, or sections 148.01 to 148.106, and an individual operating x-ray equipment for use on humans must pass an examination as specified in Minnesota Statutes, section 144.121, subdivision 5.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0575 EXAMINATION REQUIREMENTS.
Subpart 1.
Notice to individual.
Upon passing the examination, a written notice to the individual will be sent by the commissioner.
Subp. 3.
Validity standards.
An examination must meet validity standards for educational and psychological testing specified in the American Psychological Association's "Standards for Educational and Psychological Testing" (1986). The "Standards for Educational and Psychological Testing" are incorporated by reference, are not subject to frequent change, and are available at the Minnesota State Law Library at Room 625, Minnesota Judicial Center, 25 Rev. Dr. Martin Luther King Jr. Blvd., St. Paul, MN 55155.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0580 REGISTRANT REQUIREMENTS FOR OPERATORS IN FACILITIES USING X-RAY EQUIPMENT.
A registrant in a facility with x-ray equipment used on humans must ensure that:
A.
only individuals who have met the requirements in Minnesota Statutes, section 144.121, subdivision 5, are allowed to operate x-ray equipment;
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0585 EQUIVALENT EXAMINATIONS.
Subpart 1.
General.
An individual must be determined by the commissioner to have met the requirements in Minnesota Statutes, section 144.121, subdivision 5, if the individual has passed any of the examinations listed in this part.
Subp. 2.
Radiologic technologist registration examination.
If an individual has passed the radiography examination of the American Registry of Radiologic Technologists, the individual must be determined to have met the requirements in Minnesota Statutes, section 144.121, subdivision 5.
Subp. 3.
Chiropractic radiologic technologist registration examination.
If an individual has passed the radiography examination of the American Chiropractic Registry of Radiologic Technologists, the individual must be determined to have met the requirements in Minnesota Statutes, section 144.121, subdivision 5.
Subp. 4.
License from other United States jurisdictions.
If an individual has passed a full or limited license examination in radiography from other United States jurisdictions, the individual may request that the commissioner review the license examination to determine if the license examination is equivalent to the examination described in Minnesota Statutes, section 144.121, subdivision 5. If the examination meets the requirements of Minnesota Statutes, section 144.121, subdivision 5, the individual must be determined by the commissioner to have met the requirements of this part.
Subp. 5.
Other professional registrations.
If an individual has passed a registration examination other than one specified in this part, or an examination not approved under part 4732.0580, the individual may request a determination of equivalency according to the procedures and criteria in Minnesota Statutes, section 144.121, subdivision 5.
Subp. 6.
Physician assistants.
Physician assistants registered under Minnesota Statutes, chapter 147A, can operate equipment only as delegated by the supervising physicians in the supervisory agreement.
Subp. 7.
Examination for dual modality studies.
Individuals who have passed the nuclear medicine examination of the American Registry of Radiologic Technologists or the examination of the Nuclear Technology Certification Board meet the requirements in Minnesota Statutes, section 144.121, subdivision 5, for the purpose of operating PET/CT in nuclear medicine procedure provided they have received specific training in CT operations.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0590 INDIVIDUALS OPERATING X-RAY EQUIPMENT DURING TRAINING.
Subpart 1.
Exemptions from x-ray machine operator's exam.
An individual participating in an approved training course for physicians, dentists, chiropractors, podiatrists, radiologic technologists, chiropractic radiologic technologists, dental hygienists, or dental assistants is exempt from the requirements of part 4732.0570 for the duration of the training course. The exemption applies to activities conducted within the scope of the training course. If an individual is operating x-ray equipment for use on humans outside the scope of the training course, the individual must comply with part 4732.0570.
Subp. 2.
Externships.
If the approved program or approved course uses externships as part of the practical training, the program or course must notify the commissioner of the externship sites and dates the site is to be used. The program or course must ensure the exposure of humans to radiation during that period of training is as low as reasonably achievable and the radiation doses do not exceed the limits in parts 4732.0410 to 4732.0430.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
REPORTS AND NOTIFICATIONS
4732.0600 REPORTS OF THEFT OR LOSS OF RADIATION-PRODUCING EQUIPMENT.
Subpart 1.
Telephone reports.
A registrant must report to the commissioner the theft or loss of any radiation-producing equipment immediately after the theft or loss becomes known. The report must be made by telephone or facsimile.
Subp. 2.
Written follow-up reports.
A registrant that is required to make a report by telephone or facsimile must, within 30 days after making the telephone report, make a written report to the commissioner listing the following information:
A.
a description of the registered source of radiation involved, including the manufacturer, model, and serial number;
C.
actions that have been taken, or will be taken, to recover the radiation-producing equipment; and
D.
procedures or measures that have been, or will be, adopted to ensure against a recurrence of the loss or theft of registered equipment.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0610 REPORTS OF MEDICAL EVENTS OR INCIDENTS INVOLVING RADIATION-PRODUCING EQUIPMENT.
Subpart 1.
Notification within 24 hours.
A registrant possessing any radiation-producing equipment must notify the commissioner within 24 hours of discovering any medical event.
Subp. 2.
Additional reports.
In addition to any notification required by subpart 1, the registrant must submit a written report within 30 days to the commissioner to include:
Subp. 3.
Notification of occupational levels exceeded.
A registrant must notify the commissioner of any individual worker who was exposed beyond the worker's occupational dose under part 4732.0410 within 30 days of discovery. The registrant must notify the individual and provide a copy of the report. The information reported must include the dose data and results obtained under this chapter, as shown in records maintained by the registrant according to part 4732.0440, subpart 10. Each notification and report must:
B.
include appropriate identifying data, including the name of the registrant, the name of the exposed individual worker, and the date of the dose.
Subp. 4.
Notification of a fluoroscopic event.
Each facility using fluoroscopic equipment for interventional or special procedures must have available a record of patient exposure received per procedure for the commissioner's review. A patient's skin entrance exposure dose that exceeds 600 rads (6,000 milliGray) must be reviewed by the facility's radiation safety committee (RSC). If a facility does not have a radiation safety committee, the registrant must provide the commissioner within 30 days of the event, documentation stating why the patient's dose exceeded 600 rads (6,000 milliGray). In addition, if the patient's entrance exposure dose exceeds 600 rads (6,000 milliGray), the RSC or registrant must have an established policy and procedure to ensure appropriate potential skin injury and follow-up information is given to the patient.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0620 WARNING AND CONTROL DEVICES FOR HIGH AND VERY HIGH RADIATION AREAS.
Subpart 1.
Entrance or access points.
Each entrance or access point to a high or very high radiation area must be:
A.
equipped with a control device that causes the level of radiation to be reduced so that an individual cannot receive a dose in excess of 100 millirems (1.0 mSv) in one hour upon entry into the area;
B.
equipped with a warning device that energizes a visible or audible alarm to alert an individual entering the high or very high radiation area and other nearby nonoccupationally exposed workers;
Subp. 2.
Exception.
When a high or very high radiation area is established for 30 calendar days or less, direct surveillance to prevent unauthorized entry may be substituted for the devices required by this subpart.
Subp. 3.
Egress.
The devices required by this subpart must not prevent an individual from leaving a high or very high radiation area.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0630 BYPASSING A SAFETY DEVICE.
The registrant must ensure that:
A.
a safety device or interlock is not bypassed unless written approval has been obtained from the radiation safety officer or an alternate designated by the radiation safety officer:
C.
a readily discernible sign stating "SAFETY DEVICE OR INTERLOCK NOT WORKING" must be posted on the radiation source housing and at the control panel, when a safety device is bypassed.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
CALIBRATIONS AND MEASUREMENT INSTRUMENTS
4732.0700 CALIBRATIONS.
Subpart 1.
Diagnostic radiographic system calibrations.
The registrant must ensure that corrective actions or calibrations are performed on a diagnostic radiographic system whenever that system does not meet the minimum equipment performance criteria in nationally recognized standards, such as:
Subp. 2.
Therapeutic system calibrations.
The registrant must ensure that the corrective actions or calibrations are performed on the therapeutic equipment whenever that system does not meet the minimum equipment performance criteria in nationally recognized standards, such as:
Subp. 3.
Tests after change or replacement.
Calibration or an equipment performance evaluation must be performed when there is any change or replacement of components that could cause a change in the radiation output of that system.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0710 RADIATION SURVEY OR MEASUREMENT INSTRUMENTS.
Subpart 1.
Requirements.
To ensure correct response to radiation, each radiation survey instrument must be calibrated at intervals not to exceed 24 months and after each servicing:
B.
be calibrated to accuracy within plus or minus 20 percent over the applicable range of the instrument;
D.
the calibration of any electronic equipment must be traceable to its calibration standard at the National Institute of Standards and Technology (NIST); and
E.
noninvasive kVp meters must be calibrated by the manufacturer or an accredited calibration laboratory.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
EQUIPMENT REQUIREMENTS
4732.0800 GENERAL EQUIPMENT REQUIREMENTS FOR ALL DIAGNOSTIC RADIATION-PRODUCING SYSTEMS.
Subpart 1.
Applicability.
All diagnostic radiation-producing systems must comply with nationally recognized standards, such as:
D.
all equipment manufactured before the effective date of Code of Federal Regulations, title 21, sections 1020.30 to 1020.33, must meet the requirements of a nationally recognized standard, or this chapter.
Subp. 2.
Radiation exposure x-ray control.
An x-ray control must be incorporated into each x-ray system to comply with Code of Federal Regulations, title 21, section 1020.31. In addition, the x-ray control must meet the requirements in this subpart.
A.
The exposure control switch must be a dead-man type, which requires continuous pressure to complete the exposure.
B.
Each x-ray control console other than dental intraoral systems must be located in such a way as to meet the requirements in subitems (1) to (3).
(1)
Stationary x-ray systems must have the x-ray control permanently mounted behind the protective barrier so that the operator remains behind the barrier during the entire exposure.
(2)
Portable x-ray systems that produce more than 25 milliampere-minutes per week at the same location must meet the requirement of subitem (1).
(3)
Portable x-ray systems that produce less than 25 milliampere-minutes per week at the same location, must meet the requirement of subitem (1), or have a 6.5 foot (2.0 m) high lead equivalent protective barrier which is placed at least six feet (1.8 m) from the tube housing assembly and at least six feet (1.8 m) from the patient.
C.
The x-ray control console must provide visual indication observable at or from the operator's protected position whenever x-rays are produced.
D.
The control panel containing the main power switch must bear the warning statement which is legible and accessible to view: "WARNING This x-ray unit may be dangerous to patient and operator unless safe exposure factors, operating instructions, and maintenance schedules are observed."
E.
Any deviation of technique factors for kVp must be those specified by the manufacturer. For other technique factors, the deviation must have a coefficient of variation of no more than five percent.
F.
The x-ray control console must provide a signal audible to the operator that the exposure has terminated.
G.
Automatic or semiautomatic collimators (PBL) may be permanently changed to a manual mode, if the facility chooses. This requires the automatic system to be permanently disabled. The collimator must be relabeled with a durable sign that is clearly observable to the operator that states "manual operation required."
Subp. 3.
Radiation exposure automatic exposure controls.
When an automatic exposure control is provided, the control must meet Code of Federal Regulations, title 21, section 1020.31.
Subp. 4.
Radiation from capacitor energy storage equipment.
Radiation emitted from the x-ray tube must comply with Code of Federal Regulations, title 21, section 1020.31.
Subp. 5.
Diagnostic radiographic systems designed for one image receptor size.
These systems must meet Code of Federal Regulations, title 21, section 1020.31.
Subp. 6.
Beam quality, half-value layer.
The half-value layer of the useful beam for a given kVp must not be less than the values shown in item A. If it is necessary to determine a half-value layer at a kVp, which is not listed in item A, linear interpolation or extrapolation may be made.
A.
Values for half-value layer of useful beam for x-ray tube:
| Design operating range (kVp) | Measured kVp | Half-value layer (millimeter of aluminum) Other x-ray Systems* |
Specified Dental Systems |
| Below 50 | 30 | 0.3 | 1.5 |
| 40 | 0.4 | 1.5 | |
| 50 | 0.5 | 1.5 | |
| 51-70 | 51 | 1.2 | 1.5 |
| 60 | 1.3 | 1.5 | |
| 70 | 1.5 | 1.5 | |
| Above 70 | 71 | 2.1 [2.5] | 2.1 |
| 80 | 2.3 [2.9] | 2.3 | |
| 90 | 2.5 [3.2] | 2.5 | |
| 100 | 2.7 [3.6] | 2.7 | |
| 110 | 3.0 [3.9] | 3.0 | |
| 120 | 3.2 [4.3] | 3.2 | |
| 130 | 3.5 [4.7] | 3.5 | |
| 140 | 3.8 [5.0] | 3.8 | |
| 150 | 4.1 [5.4] | 4.1 |
*Systems manufactured after June 10, 2006, are in brackets. All other systems were manufactured before June 10, 2006.
B.
All intraoral dental radiographic systems installed on and after December 1, 1980, must have a minimum half-value layer not less than 1.5 millimeters aluminum.
C.
For capacitor energy storage equipment, compliance with the requirements of this subpart must be determined with the capacitors fully charged and with a technique that discharges at least half of the energy stored in the capacitors, half of the maximum milliampere-second.
D.
The half-value layer of the useful beam must be measured with all the materials in the beam that normally are present between the source and the patient.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0820 GENERAL PURPOSE DIAGNOSTIC RADIATION-PRODUCING EQUIPMENT MANUFACTURED BEFORE 1973.
Subpart 1.
Applicability.
Diagnostic radiation-producing equipment in veterinary facilities or equipment manufactured before 1973 must meet the requirements of the manufacturer's specifications or the requirements in this part in addition to other requirements in this chapter.
Subp. 2.
Beam limitation.
The useful beam must be limited to the patient's area of clinical interest.
A.
Means must be provided to limit the x-ray field in the plane of the image receptor so the field does not exceed each dimension of the image receptor by more than two percent of the SID when the axis of the x-ray beam is perpendicular to the plane of the image receptor.
B.
Means must be provided to align the center of the x-ray field with the center of the image receptor to within two percent of the SID, or means must be provided to align the x-ray field so the x-ray field at the plane of the image receptor does not extend beyond any edge of the image receptor.
C.
The requirements of items A and B may be met with either:
(1)
an assortment of removable, fixed-aperture, beam-limiting devices sufficient to meet the requirement for each combination of image receptor size and SID for which the system is designed with each device having clear and permanent markings to indicate the image receptor size and SID for which it is designed; or
(2)
a beam-limiting device having multiple fixed apertures sufficient to meet the requirement for each combination of image receptor size and SID for which the system is designed. Permanent, clearly legible markings must indicate the image receptor size and SID for which each aperture is designed and must indicate which aperture is in position for use.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0825 FLUOROSCOPIC X-RAY SYSTEMS EXCEPT RADIATION THERAPY SIMULATORS.
Subpart 1.
Applicability.
All fluoroscopic systems must meet the requirements in this chapter and the applicable performance standards of nationally recognized standards, such as:
Subp. 2.
Fluoroscopic training requirements.
Except licensed practitioners of the healing arts, any individual activating the fluoroscopic system must be trained in the aspects of fluoroscopic equipment use listed in items A to J. The topics to be covered and documented are:
Subp. 3.
Registrant requirements.
The registrant must ensure that:
A.
the written safety procedures provide precautionary measures to be adhered to when image intensified fluoroscopes are used for specific surgical applications;
B.
portable fluoroscopic equipment must have spacer cones and the spacer cones must remain with the portable fluoroscopic equipment at all times. Appropriate spacer cones must be placed on the portable fluoroscopic equipment that is used outside of the surgical setting;
C.
any individual who is in the room during a fluoroscopic procedure must wear a protective garment of not less than 0.5 millimeter lead equivalence; and
D.
all fluoroscopic x-ray equipment must be provided with a bucky-slot cover panel, if applicable, and either lead drapes attached to the intensifying tower or self-supporting shields of not less than 0.5 millimeter lead equivalent material.
Subp. 4.
Limitation of useful beam x-ray field.
A.
All fluoroscopic systems must be provided with image intensification equipment to view the fluoroscopic images.
B.
Spot-film devices must meet the field limitation and alignment requirements in Code of Federal Regulations, title 21, section 1020.31.
Subp. 5.
Entrance exposure rate allowable limits.
Fluoroscopic systems must meet requirements in Code of Federal Regulations, title 21, section 1020.32.
A.
Fluoroscopic equipment with automatic exposure rate control (AERC) must not be operable at any combination of tube potential and current that results in an air kerma rate in excess of ten roentgens per minute or 2.58 x 10-3 C/kg per minute at the point where the center of the useful beam enters the patient, except:
(2)
when an optional high-level control is provided. When so provided, the equipment must not be operable at any combination of tube potential and current that results in an air kerma rate in excess of five R/min (1.29 x 10-3 C/kg per minute) at the point where the center of the useful beam enters the patient, unless the high-level control is activated. Special means of activation of high-level controls is required. The high-level control must be operable only when the operator provides continuous manual activation. A continuous signal audible to the fluoroscopist must indicate that the high-level control is being employed.
B.
Fluoroscopic equipment without AERC (manual mode) must not be operable at any combination of tube potential and current that results in an air kerma rate in excess of five R/min (1.29 x 10-3 C/kg per minute) at the point where the center of the useful beam enters the patient:
(2)
when an optional high-level control is activated. Special means of activation of high-level controls is required. The high-level control must be operable only when the operator provides continuous manual activation. A continuous signal audible to the fluoroscopist must indicate that the high-level control is being employed.
C.
Fluoroscopic equipment with both an AERC mode and a manual mode must not be operable at any combination of tube potential and current that results in an air kerma rate in excess of ten R/min (2.58 x 10-3 C/kg per minute) in either mode at the point where the center of the useful beam enters the patient, except:
(2)
when the mode or modes have an optional high-level control, in which case that mode or modes must not be operable at any combination of tube potential and current that results in an air kerma rate in excess of five R/min (1.29 x 10-3 C/kg per minute) at the point where the center of the useful beam enters the patient, unless the high-level control is activated. Special means of activation of high-level controls is required. The high-level control must be operable only when the operator provides continuous manual activation.
D.
The registrant with fluoroscopic systems manufactured after May 19, 1995, must ensure that the entrance exposure rate allowable limits in this subpart are met.
(1)
Fluoroscopic equipment operable at any combination of tube potential and current that results in an air kerma rate greater than five R/min (1.29 x 10-3 C/kg per minute) at the point where the center of the useful beam enters the patient must be equipped with automatic exposure rate control. Provision for manual selection of technique factors may be provided.
(2)
Fluoroscopic equipment must not be operable at any combination of tube potential and current that results in an exposure rate in excess of ten R/min (2.58 x 10-3 C/kg per minute) at the point where the center of the useful beam enters the patient, except:
(a)
during the recording of images from an x-ray image-intensifier tube using photographic film; or
(b)
when an optional high-level control is activated, the equipment must not be operable at any combination of tube potential and current that results in an air kerma rate in excess of 20 R/min (5.16 x 10-3 C/kg per minute) at the point where the center of the useful beam enters the patient. Special means of activation of high-level control is required. The high-level control must only be operable when the operator provides continuous manual activation. A continuous signal audible to the fluoroscopist must indicate that the high-level control is being employed.
Subp. 6.
Indication of kilovoltage and milliamperage.
For fluoroscopic x-ray systems, kilovoltage and the milliamperage must be continuously indicated.
Subp. 7.
Source-to-skin distance.
The source-to-skin distance must not be less than:
D.
7.9 inches (20 centimeters) for image intensified fluoroscopes used for specific surgical applications.
Subp. 8.
Control of scattered radiation.
The procedures in this subpart must be used to control scattered radiation from all fluoroscopes.
A.
When a fluoroscopic table with an under table x-ray tube is used, the bucky opening must be shielded to attenuate the scattered radiation by at least 70 percent. Lead drapes must be attached to the intensifier tower to attenuate scattered radiation by at least 70 percent.
B.
For other under table configurations, provisions must be made through equipment design or radiation protection measures to ensure that individuals do not receive a dose in excess of the allowable dose limits listed in parts 4732.0410 to 4732.0430.
C.
For single-tube above table combination radiographic and fluoroscopic x-ray systems used in the fluoroscopic mode, protective aprons of not less than 0.5 millimeter lead equivalence must be used to ensure that any individual who is in the room during a fluoroscopic procedure does not receive a dose greater than the allowable dose limits in part 4732.0410. In addition, portable lead shields, barriers, or aprons of not less than 0.5 millimeter lead equivalence must be used.
D.
For portable C-arm fluoroscopes, provisions must be made through the use of protective aprons of not less than 0.5 millimeter lead equivalence to ensure that any individual other than the patient who may be exposed during a fluoroscopic procedure does not receive a dose in excess of the allowable dose limits in part 4732.0410.
Subp. 9.
Radiation therapy simulation systems.
A radiation therapy simulation system is exempt from the requirements of subpart 3, provided:
A.
the system is designed and used so that no individual other than the patient is in the simulation room when the system is producing x-rays; and
B.
the system has a means to indicate the cumulative time that an individual patient has been exposed to x-rays. Procedures must require in such cases that the timer be reset between examinations.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0830 FLUOROSCOPIC DOSE-AREA-PRODUCT MONITOR.
All fluoroscopic equipment installed 90 days after November 5, 2007, must be equipped with a dose-area-product monitor or comparable device, capable of recording the total radiation dose received by a patient when the fluoroscopic tube is used.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0835 REQUIREMENTS FOR COMPUTED RADIOGRAPHY, DIGITAL RADIOGRAPHY, OR PHOTOSTIMULABLE STORAGE PHOSPHOR RADIATION-PRODUCING EQUIPMENT.
Subpart 1.
Requirements.
Persons registered to possess radiation-producing equipment must be responsible for maintaining equipment in compliance with this chapter and:
Subp. 2.
Applicability.
Facilities that have radiation-producing equipment that is filmless, photostimulable storage phosphor, computed radiography, or digital radiography must comply with this part and other pertinent requirements in this chapter.
Subp. 3.
Registrant requirements.
The registrant using computed radiography, digital radiography, or photostimulable storage phosphor radiation-producing equipment must ensure that:
B.
occupational dose and dose to the public limits in parts 4732.0410 to 4732.0430 are not exceeded;
C.
equipment calibration tests at the time of installation and equipment performance evaluations are conducted at intervals not to exceed 24 months according to:
(1)
a nationally recognized standard, such as Code of Federal Regulations, title 21, section 1020;
E.
individuals who will be operating or maintaining the radiation-producing equipment meet the requirements in Minnesota Statutes, section 144.121, subdivision 5, and:
(1)
have taken the required training by the equipment manufacturer or the equivalent on the use of the equipment and the training is documented; and
(2)
are adequately instructed initially in site-specific operating and emergency procedures and the training is documented; and
F.
a technique chart is used for all radiographic exposures. The technique chart must reflect the technique parameters for the individual system.
Subp. 4.
Quality assurance or quality control procedures.
The registrant must ensure that:
A.
all quality assurance or quality control procedures must be established by the registrant, recommended by a nationally recognized professional organization, or be recommended by the manufacturer;
B.
the quality assurance or quality control procedure frequency, corrective actions taken, and date and initials of the individual completing the procedures are documented and maintained at the site; and
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0850 BONE DENSITOMETRY SYSTEMS.
Subpart 1.
Applicability.
Facilities using bone densitometry systems or pQCT peripheral systems must comply with the requirements in this part and other relevant requirements in this chapter. Persons registered to possess radiation-producing equipment must be responsible for maintaining the equipment in compliance with:
Subp. 2.
General requirements for bone densitometry systems.
The registrant must ensure that:
A.
systems with stepless collimators are provided with the means to both size and align the x-ray field at the place of the image receptor and does not exceed the SID by two percent;
B.
during the operation of the bone densitometry system, the operator, ancillary personnel, and members of the general public must be positioned to maintain occupational radiation dose and dose to the public as low as reasonably achievable during the examination so as not to exceed the limits in parts 4732.0410 to 4732.0430;
Subp. 3.
Quality assurance or quality control procedures.
The registrant must ensure that:
A.
all quality assurance or quality control procedures follow the recommendations of a nationally recognized standard, and the manufacturer's specifications for quality control tests;
B.
the frequency of quality assurance or quality control procedures, and corrective actions taken as a result of the quality control testing are followed and documented; and
C.
the facility's operating and emergency procedures include quality assurance or quality control procedures.
Subp. 4.
Bone density system operators.
The registrant must ensure that an operator of bone densitometry equipment must:
A.
be a licensed practitioner of the healing arts, physician assistant, registered radiologist assistant or radiology practitioner assistant, or be an x-ray operator having fulfilled the requirements of Minnesota Statutes, section 144.121, subdivision 5;
B.
complete specific manufacturer's training or the equivalent on bone densitometry equipment; and
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0860 COMPUTED TOMOGRAPHY REQUIREMENTS.
Subpart 1.
Applicability.
A.
All computed tomography systems must meet the requirements of:
(1)
nationally recognized standards such as Code of Federal Regulations, title 21, section 1020.33;
B.
Computed tomography facilities must meet the requirements in this part and other pertinent requirements in this chapter.
Subp. 2.
Facility design requirements.
A.
The control panel must be mounted in a permanently protected area outside the computed tomography room meeting the requirements in part 4732.0355, subpart 4.
B.
If the control booth is located within the CT room, the control booth must meet the requirements of part 4732.0355, subpart 4.
C.
In either case, the operator is required to remain in that protected area during the entire exposure.
Subp. 3.
Viewing systems.
A.
Windows, mirrors, closed-circuit television, or an equivalent must be provided to permit continuous operator observation of the patient from the control panel during irradiation.
B.
When the primary viewing system is by electronic means, an alternate viewing system must be available for use in the event of failure of the primary viewing system.
Subp. 4.
Audio communication.
Provision must be made for two-way audio communication between the patient and operator at the control panel.
Subp. 5.
Radiation surveys.
All computed tomography systems installed 90 days after November 5, 2007, and those systems not previously surveyed, must have a radiation survey made to identify radiation levels at the control panel and spaces adjoining the room. In addition, the radiation surveys must be completed after any change in the facility or equipment which might cause a significant increase in radiation hazard. The radiation survey must be maintained by the registrant according to part 4732.0330.
Subp. 6.
Equipment performance measurements.
A.
The registrant must ensure that the equipment performance measurement procedures in this part are performed at intervals not to exceed 24 months according to:
B.
The equipment performance measurement of the radiation output of the CT x-ray system must be performed by a registered service provider.
C.
The equipment performance measurements of a CT system must be performed at intervals not to exceed 24 months or after change or replacement of components that could cause an increase in radiation hazard or that could result in the minimum performance criteria in part 4732.1100 not being met.
D.
The measurements of the radiation output of a CT system must be performed with a calibrated dosimetry system. The calibration of such system must be traceable to a national standard. The dosimetry system must have been calibrated within the preceding 24 months.
E.
CT dosimetry phantoms must be used in determining the radiation output of a CT system. The phantoms must comply with Code of Federal Regulations, title 21, section 1020.33.
F.
The computed tomography dose index (CTDI) must be completed using the CT dosimetry phantom. For the purpose of determining the CTDI, the manufacturer's statement as to the nominal tomographic section thickness for that particular system may be used.
G.
The dose measurements must be made for standard head and body scan modes of operation used at the facility.
H.
The image quality measurements must be made using a typical clinical technique in the standard head and body scan modes of operation.
Subp. 7.
Spot checks.
The registrant must ensure the spot checks for the computed tomography equipment specified in this part are performed at intervals not to exceed 12 months to verify the system's integrity.
A.
The spot check procedures must be written procedures developed by the manufacturer or a registered service provider.
B.
The spot check procedures must incorporate the use of a CT image quality phantom to provide an indication of contrast scale, noise, nominal tomographic section thickness, the resolution capability of the system for low and high contrast objects, and measuring the mean computed tomography noise (CTN) for water or other reference material.
C.
Spot checks must include acquisition of images obtained with the CT image quality phantoms using the same processing mode and CT conditions of operation as are used to perform equipment performance measurements in part 4732.1100. The images must be maintained, until a new equipment performance test is performed.
Subp. 8.
Equipment performance measurements performed by the CT operator.
In addition to the equipment performance measurements in subpart 6, an operator must:
Subp. 9.
Program review.
The registrant or radiation safety officer must review, sign, and date the operator's equipment performance measurements at least quarterly.
Subp. 10.
Operating procedures.
Information about the operation, radiation surveys, and equipment performance measurements of the system must be available for the employees and for the commissioner at the time of an inspection. The registrant must ensure that:
A.
the CT system is operated by an individual who:
(1)
after January 1, 2008, is a licensed practitioner of the healing arts, or individuals who meet the requirements in Minnesota Statutes, section 144.121, subdivision 5;
(3)
has had training in appropriate CT positioning and anatomy for procedures performed at the facility; and
B.
information about the system must be available at the control panel regarding the operation. The information must include the following:
(1)
a current technique chart available at the control panel, which specifies for each routine examination the CT conditions of operation and the number of scans per examination; and
(2)
instructions on the use of the CT dosimetry or image quality phantoms including the allowable variations for the indicated parameters.
Subp. 11.
Corrective actions.
A.
Correction of the problem must take place and be verified by performing the equipment performance measurements according to Code of Federal Regulations, title 21, section 1030, the manufacturer's specifications, or part 4732.1100.
B.
Corrective action must take place if the equipment performance measurements or spot checks of the CT system indicate that a system operating parameter has exceeded a tolerance established:
(3)
by a registered service provider.
When an operating parameter has been exceeded, the CT system equipment on patients must not be used or must be limited to those uses permitted by established written instructions until the corrective actions have been taken and verification of the correction has been made and documented.
Subp. 12.
CT fluoroscopic procedures.
If the equipment has the capabilities of performing fluoroscopic procedures, the x-ray control may be operated in the CT room and essential personnel may remain in the room during the fluoroscopic procedures provided they:
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0865 COMPUTERIZED TOMOGRAPHY DESIGNED FOR VISUALIZATION OF THE HEAD AND SOFT TISSUE OF THE NECK.
Subpart 1.
Applicability.
Computed tomography systems designed for visualization of head and soft tissues of the neck must meet requirements of this chapter and:
Subp. 2.
Facility design requirements.
A.
The control panel must be mounted in a permanently protected area outside the computed tomography room and meet the requirements of part 4732.0355, subpart 2.
B.
If the control area is within the CT room, the requirements for a control booth in part 4732.0355, subpart 2, must be followed.
D.
Viewing systems must be windows, mirrors, closed-circuit television, or an equivalent able to provide continuous operator observation of the patient from the control panel during irradiation.
E.
Provision must be made for two-way audio communication between the patient and operator at the control panel.
Subp. 3.
Radiation surveys.
All computed tomography systems installed 90 days after November 5, 2007, and those systems not previously surveyed, must have a radiation survey to identify radiation levels at the control panel and the spaces adjoining the CT room. In addition, the surveys must be completed after any change in the facility or equipment that might cause a significant increase in radiation hazard. The survey must be maintained by the registrant according to part 4732.0330.
Subp. 4.
Equipment performance measurements.
A.
The registrant must ensure that the equipment performance measurement procedures are performed at intervals not to exceed 24 months according to:
B.
The equipment performance measurement of the radiation output of the CT x-ray system must be performed by a registered service provider.
C.
The equipment performance measurements of a CT system must be performed at intervals not to exceed 24 months or after change or replacement of components that could cause an increase in radiation hazard or that could result in the minimum performance criteria in part 4732.1100 not being met.
D.
The measurements of the radiation output of a CT system must be performed with a calibrated dosimetry system. The calibration of such system must be traceable to a national standard. The dosimetry system must have been calibrated within the preceding 24 months.
E.
CT dosimetry phantoms must be used in determining the radiation output of a CT system. The phantoms must comply with Code of Federal Regulations, title 21, section 1020.33 or equivalent phantom.
F.
The dose measurements must be made for standard head scan mode of operation used at the facility.
G.
The image quality measurements must be made using a typical clinical technique in the standard head scan mode of operation.
Subp. 5.
Spot checks.
The registrant must ensure the spot checks for the computed tomography equipment in this part are performed at intervals not to exceed 12 months to verify the system's integrity.
A.
The spot check procedures must be written procedures developed by the manufacturer or a registered service provider.
B.
All spot checks must be included in the equipment performance measurements and at time intervals and system conditions specified by the manufacturer or a registered service provider.
C.
The spot check procedures must incorporate the use of a CT image quality phantom to provide an indication of contrast scale, noise, the resolution capability of the system for low and high contrast objects, and must measure the mean computed tomography noise (CTN) for water or other reference material.
D.
Spot checks must include acquisition of images obtained with the CT image quality phantoms using the same processing mode and CT conditions of operation that are used to perform equipment performance measurements according to part 4732.1100. The images must be maintained until a new equipment performance test is performed.
Subp. 6.
Equipment performance measurements performed by the CT operator.
In addition to the equipment performance measurements described in subpart 4, an operator must:
Subp. 7.
Program review.
The registrant or radiation safety officer must review, sign, and date the operator's equipment performance measurements at intervals not to exceed 12 months.
Subp. 8.
Operating procedures.
The registrant must ensure that:
A.
the CT system is operated by an individual who:
(1)
after January 1, 2008, is a licensed practitioner of the healing arts, or individuals who meet the requirements in Minnesota Statutes, section 144.121, subdivision 5;
(3)
has training on appropriate positioning and anatomy for the use of the equipment in the facility; and
B.
information of the system is available at the control panel regarding the operation. The information must include the following:
(1)
a current technique chart available at the control panel, which specifies for each routine examination, the CT conditions of operation and the number of scans per examination; and
(2)
instructions on the use of the CT dosimetry or image quality phantoms including the allowable variations for the indicated parameters.
Subp. 9.
Corrective actions.
A.
Correction of the problem must take place and be verified by performing the equipment performance measurements according to:
B.
The equipment must not be used until corrective actions have been taken, verified, and documented, if the equipment performance measurement or spot check of the CT system indicates that a system operating parameter has exceeded a tolerance established:
Subp. 10.
CT fluoroscopic procedures.
If the equipment has the capabilities of performing fluoroscopic procedures, the x-ray control may be operated in the CT room and essential personnel may remain in the room during the fluoroscopic procedures provided they:
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0870 REQUIREMENTS FOR STEREOTACTIC MAMMOGRAPHIC EQUIPMENT.
Subpart 1.
Equipment requirements.
Radiation-producing equipment specifically designed to perform stereotactically guided breast biopsies must meet the requirements of this chapter and:
Subp. 2.
Registrant requirements.
The registrant must ensure that:
A.
individuals operating the equipment meet the requirements of Minnesota Statutes, section 144.121, subdivision 5, or the Food and Drug Administration's Mammographic Quality Standards Act requirements;
B.
individuals have completed equipment manufacturer's training or equivalent and initial site-specific training in the registrant's operating and emergency procedures;
D.
the entire system for stereotactic breast biopsies including the equipment performance, procedures, and records are evaluated annually by a diagnostic radiographic physicist.
Subp. 3.
Quality assurance and quality control procedures.
The registrant must ensure that:
A.
all manufacturer's quality assurance or quality control procedures follow the test procedures established by the registrant, recommendations of a nationally recognized standard, or the manufacturer's specifications;
B.
the frequency of the quality assurance or quality control procedures, and corrective actions as a result of quality control testing are followed and documented; and
C.
the facility's operating and emergency procedures include quality assurance or quality control procedures.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0875 VETERINARY MEDICAL RADIOGRAPHIC SYSTEMS.
Subpart 1.
Applicability.
A.
This part applies to x-ray systems used for diagnostic veterinary medicine radiography. The registrant must meet the requirements in this part and other pertinent requirements in this chapter, and the equipment must meet:
Subp. 2.
Beam limitation.
The useful beam must be limited to the area of clinical interest.
A.
Means must be provided to limit the x-ray field in the plane of the image receptor so the field does not exceed each dimension of the image receptor by more than two percent of the SID when the axis of the x-ray beam is perpendicular to the place of the image receptor.
B.
Means must be provided to align the center of the x-ray field with the center of the image receptor to within two percent of the SID, or means must be provided to align the x-ray field so the x-ray field at the plane of the image receptor does not extend beyond any edge of the image receptor.
C.
The requirements of items A and B may be met with either:
(1)
an assortment of removable, fixed-aperture, beam-limiting devices sufficient to meet the requirement for each combination of image receptor size and SID for which the system is designed, with each device having clear and permanent markings to indicate the image receptor size and SID for which it is designed; or the collimator must be labeled to indicate the field size and the SID for which it is designed; or
(2)
a beam-limiting device having multiple fixed apertures sufficient to meet the requirement for each combination of image receptor size and SID for which the system is designed. Permanent, clearly legible markings must indicate the image receptor size and SID for which each aperture is designed and must indicate which aperture is in position for use.
Subp. 3.
X-ray control console.
B.
The x-ray control console must provide visual indication observable from the operator's protected position whenever x-rays are produced.
C.
The x-ray control console must provide a signal audible to the operator when the exposure has terminated.
Subp. 4.
Beam quality half-value layer.
The requirements for half-value layer found in part 4732.0800, subpart 6, must be met.
Subp. 5.
Operating procedures.
The registrant must provide operating procedures to ensure that dose limits in parts 4732.0400 to 4732.0430 are not exceeded.
B.
No individual other than the operator can be in the radiographic room while exposures are being made unless the individual's assistance is required.
C.
When an animal must be held by an individual during radiography, that individual must wear protective aprons and gloves of at least 0.5 millimeters lead equivalency. The individual must be positioned so that no part of the body, protected or unprotected, will be struck by the useful beam.
D.
A mechanical cassette holding device must be used for horizontal beam x-rays whenever possible.
Subp. 6.
Additional requirements for fluoroscopic systems in veterinary facilities.
All fluoroscopic x-ray systems must be image intensified and meet the requirements in items A to J:
A.
The fluoroscopic imaging assembly must be provided with a primary protective barrier that intercepts the entire cross section of the useful beam at any SID.
B.
The x-ray tube used for fluoroscopy must not produce x-rays unless the barrier is in position to intercept the entire useful beam.
C.
For fluoroscopic systems with or without a spot film device, the length or the width of the x-ray field in the plane of the image receptor must not exceed the length or width of the visible area of the image receptor by more than three percent of the SID.
D.
For spot-film beam limitation, the x-ray field size in the plane of the film must be adjustable to a size smaller than the selected portion of the film. The minimum field size at the greatest SID must be equal to, or less than, five centimeters by five centimeters.
E.
The center of the x-ray field in the plane of the film must be aligned with the center of the selected portion of the film to within two percent of the SID.
F.
Fluoroscopic equipment that is provided with automatic exposure rate control must not be operable at any combination of kVp and mA which will result in an exposure rate in excess of ten roentgens (2.6 mC/kg) per minute at the point where the center of the useful beam enters the patient, except:
G.
Fluoroscopic equipment that is not provided with automatic exposure rate control must not be operable at any combination of kVp or mA which will result in an exposure rate in excess of five roentgens (1.3 mC/kg) per minute at the point where the center of the useful beam enters the patient, except:
H.
If a high-level control is available, a continuous signal audible to the fluoroscopist must indicate that the high-level control is being employed.
I.
X-ray production in the fluoroscopic mode must be controlled by a device that requires continuous pressure by the fluoroscopist for the entire time of any exposure.
Subp. 7.
Additional requirements for therapeutic systems in veterinary medical facilities.
Veterinary therapeutic equipment must meet the specifications in items A to C.
A.
When the x-ray tube is operated at its maximum rated mA for the maximum kV, the leakage air kerma rate must not exceed the following value:
(1)
150 kV systems: the leakage air kerma rate measured at any position five centimeters from the tube housing assembly must not exceed 100 mrad (1 mGy) in any one hour;
(2)
systems greater than 150 kV and less than 500 kV systems: the leakage air kerma rate measured at a distance of one meter from the target in any direction must not exceed one rad (1 cGy) in any one hour.
B.
A suitable irradiation timer control device must be provided to terminate the irradiation after a preset time interval.
C.
The control panel, in addition to the displays, must have an indication of whether electrical power is available at the control panel and if activation of the x-ray tube is possible; and:
Subp. 8.
Additional requirements for dental intraoral systems in veterinary medical facilities.
Veterinary dental intraoral equipment must:
A.
be provided with a position-indicating device to limit source-to-skin distance to not less than 7.1 inches (18 centimeters);
B.
employ collimation to limit the x-ray field such that:
(1)
if the minimum source-to-skin distance is 7.1 inches (18 centimeters) or more, the x-ray field, at the minimum, must be containable in a circle having a diameter of no more than 2.76 inches (seven centimeters); or
(2)
with rectangular position-indicating devices, the longer side must not exceed two inches (5.1 centimeters); and
C.
be such that the tube housing and position-indicating device must be stable before and during the exposure. The tube housing cannot be hand-held during an exposure.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0880 INTRAORAL DENTAL RADIOGRAPHIC SYSTEMS.
Subpart 1.
Applicability.
This part applies to intraoral dental radiographic systems. The dental intraoral x-ray systems must meet the requirements of:
A.
nationally recognized standards such as Code of Federal Regulations, title 21, sections 1020.31 to 1020.33;
Subp. 2.
Safety controls.
The registrant must ensure that the safety controls in this subpart are followed.
A.
Intraoral film holders and bite blocks must be used except when endodontic procedures do not permit.
C.
The tube housing and the position-indicating device must not be hand-held during an exposure and must be stable before the exposure is initiated and during the exposure.
D.
The exposure at the end of the cone for a posterior bitewing technique must not exceed the values listed in the table below:
| kVp | "D" Speed Film ESE (milliroentgens) | "E," D/E, or E+ Speed Film ESE (milliroentgens) |
| 50 | 425 - 575 | 220 - 320 |
| 55 | 350 - 500 | 190 - 270 |
| 60 | 310 - 440 | 165 - 230 |
| 65 | 270 - 400 | 140 - 200 |
| 70 | 240 - 350 | 120 - 170 |
| 75 | 170 - 260 | 100 - 140 |
| 80 | 150 - 230 | 90 - 120 |
| 85 | 130 - 200 | 80 - 105 |
| 90 | 120 - 180 | 70 - 90 |
| 95 | 110 - 160 | 60 - 80 |
| 100 | 100 - 140 | 50 - 70 |
(2)
the indicated kVp is often significantly different from the actual kVp. The kVp must be tested at the time the output per film is measured to determine the correct exposure range to be applied.
E.
The operator of the radiographic equipment must be protected and able to view the patient during the taking of any radiographs.
Subp. 3.
Beam quality half-value layer.
The requirements for half-value layer found in part 4732.0800, subpart 6, must be met.
Subp. 4.
Digital radiography.
In addition to the requirements of this part, the exposure at the end of the cone of digital dental radiographic equipment must not exceed 120 mR for a posterior bitewing.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0890 EXTRAORAL DENTAL SYSTEMS.
Subpart 1.
Requirements.
X-ray systems used for extraoral dental radiography must meet the requirements in this chapter and in:
Subp. 2.
Safety controls.
The registrant must ensure that the following safety controls are followed:
C.
the operator of the radiation-producing equipment must be protected and able to view the patient during the taking of any radiographs; and
Subp. 3.
Quality assurance and quality control procedures.
The registrant must ensure that:
A.
quality assurance or quality control procedures follow the test procedures established by the registrant, recommendations of a nationally recognized professional organization, or the manufacturer's specifications; and
B.
quality assurance or quality control procedures are completed at the required frequency, corrective actions are taken, and verification tests are accomplished as applicable.
Subp. 4.
Digital radiography.
For digital radiography, the registrant must ensure that, in addition to the requirements of this part, the following requirements are met:
A.
the radiation-producing equipment must be used according to a nationally recognized standard, the manufacturer's specifications, or part 4732.1100; and
B.
the technique chart used for all radiographic exposures reflects the technique parameters for the individual system.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0895 DENTAL COMPUTED TOMOGRAPHY SYSTEMS.
Refer to part 4732.0865, computerized tomography designed for visualization of the head and soft tissues of the neck.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
RADIATION THERAPEUTIC REQUIREMENTS
4732.0900 GENERAL REQUIREMENTS FOR FACILITIES USING ACCELERATORS.
Subpart 1.
Applicability.
Facilities using accelerators must comply with the requirements in this part and other pertinent requirements in this chapter.
Subp. 2.
Operations.
A.
A registrant shall not permit an individual to act as an operator of an accelerator until the individual:
(1)
has been instructed in radiation safety and has demonstrated an understanding of radiation safety;
(2)
has received copies of and instruction in the applicable requirements of this chapter, the registrant's operating and emergency procedures, and demonstrated an understanding of these requirements and procedures;
(3)
has demonstrated competence in the use of the accelerator, related equipment, and the radiation survey instruments employed.
B.
In addition to the audit required in part 4732.0535, each operator's performance during an actual accelerator operation must be audited by the radiation safety officer or designee at intervals not to exceed 12 months. If an operator has not participated in an accelerator operation for more than six months since the last audit, the individual's performance must be observed and recorded at the first opportunity the individual participates in an accelerator operation.
Subp. 3.
Radiation safety officer duties for accelerator facilities.
In addition to the requirements in part 4732.0505, a radiation safety officer's duties include, but are not limited to, the duties in items A to L. The radiation safety officer must:
B.
review the established procedures regularly to ensure that the procedures are current and conform to this chapter;
C.
oversee and approve all phases of the training program for accelerator operators so that appropriate and effective radiation protection practices are taught;
D.
ensure that personnel are complying with this chapter and the operating and emergency procedures;
F.
assume control and institute corrective actions including shutdown of operations when necessary in emergency situations or unsafe conditions;
G.
ensure that inspection and maintenance programs are performed according to this part and the manufacturer's specifications;
J.
ensure that any required interlock switches and warning signals are functioning and that radiation signs, ropes, and barriers are properly posted and positioned;
K.
investigate and report to the commissioner each known or suspected case of radiation exposure to an individual or radiation level detected in excess of limits established by this chapter, to determine the cause, and to take steps to prevent its recurrence; and
Subp. 4.
Individual monitoring.
In addition to the requirements of part 4732.0440, individual monitoring devices must be required for all individuals entering any area for which interlocks are required unless:
A.
a radiation survey of that area has determined that radiation levels are below that of a high radiation area; and
Subp. 5.
Operating and emergency procedures.
B.
Unless otherwise specified in this chapter, all safety and warning devices, including interlocks, must be checked for proper operation at intervals not to exceed three months. Results of these tests must be maintained at the accelerator facility for inspection by the commissioner according to part 4732.0330.
D.
A copy of the current operating and emergency procedures must be maintained at the accelerator control panel.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0925 GENERAL REQUIREMENTS FOR THERAPEUTIC EQUIPMENT.
Subpart 1.
Protection radiation survey measurements.
A.
The registrant must ensure that facility radiation surveys required by part 4732.0380, subpart 4, are performed with the therapeutic radiation machine in a "BEAM-ON" condition, with the largest clinically available treatment field and with a scattering phantom in the useful beam of radiation.
B.
The registrant must ensure that equipment quality control measurements are performed at intervals not to exceed 12 months.
Subp. 2.
Dosimetry equipment.
A.
The registrant must have a calibrated dosimetry system available for quality control measurements. The system must be calibrated by the National Institute for Standards and Technology (NIST) or by an American Association of Physicists in Medicine (AAPM) Accredited Dosimetry Calibration Laboratory (ADCL). The calibration must have been performed within the previous 24 months and after any servicing that may have affected system calibration.
(1)
For beams with energies greater than one MV (one MeV), the dosimetry system must have been calibrated for Cobalt-60.
(2)
For beams with energies equal to or less than one MV (one MeV), the dosimetry system must have been calibrated at an energy (energy range) appropriate for the radiation being measured.
B.
The dosimetry system may be compared with a system that has been calibrated according to this subpart. This comparison must have been performed within the previous 12 months and after each servicing that may have affected system calibration. The quality control check system may be the same system used to meet the requirements in this subpart.
C.
The registrant must maintain a record of each dosimetry system calibration, intercomparison, and comparison for the duration of the license or registration. For each calibration, intercomparison, or comparison, the record must include:
(2)
the model numbers and serial numbers of the instruments that were calibrated, intercompared, or compared;
(4)
the names of the individuals who performed the calibration, intercomparison, or comparison; and
(5)
evidence that the intercomparison was performed by, or under the direct supervision and in the physical presence of, a therapeutic radiological physicist.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0930 THERAPEUTIC RADIATION MACHINES OF LESS THAN 500 KV.
Subpart 1.
Equipment requirements.
A.
When the x-ray tube is operated at its maximum rated tube current for the maximum kV, the leakage air kerma rate must not exceed the value specified at the distance specified for that classification of therapeutic radiation machine.
B.
For 150 kV systems, the leakage air kerma rate measured at any position five centimeters from the tube housing assembly must not exceed 100 mrad (one mGy) in any one hour.
C.
For systems greater than 150 kVp and less than 500 kV, the leakage air kerma rate measured at a distance of one meter from the target in any direction must not exceed one rad (one cGy) in any one hour. This air kerma rate measurement may be averaged over areas no larger than 100 square centimeters. In addition, the air kerma rate at a distance of five centimeters from the surface of the tube housing assembly must not exceed 30 rad (30 cGy) per hour.
D.
For each therapeutic machine, the registrant must determine, or obtain from the manufacturer, the leakage radiation existing for the specified operating conditions.
E.
The registrant must maintain the records on leakage radiation measurements at the facility according to part 4732.0330.
F.
Permanent diaphragms or cones used for limiting the useful beam must provide at least the same degree of attenuation as required for the tube housing assembly.
G.
Adjustable or removable beam-limiting devices, diaphragms, cones, or blocks must not transmit more than five percent of the useful beam for the most penetrating beam used. When adjustable beam-limiting devices are used, the position and shape of the radiation field must be indicated by a light beam.
H.
The filter system must be designed so that:
(2)
for equipment installed after July 9, 1997, an interlock system prevents irradiation if the proper filter is not in place;
(3)
the air kerma rate escaping from the filter slot must not exceed one rad (one cGy) per hour at one meter under any operating conditions; and
I.
The x-ray tube must be mounted so that it cannot accidentally turn or slide with respect to the housing aperture. The tube housing assembly must be capable of being immobilized for stationary portal treatments.
J.
The tube housing assembly must be so marked that it is possible to determine the location of the source to within five millimeters, and such marking must be readily accessible for use during calibration procedures.
K.
Contact therapy tube housing assemblies must have a removable shield equivalent in attenuation to 0.5 millimeters of lead at 100 kV, which can be positioned over the entire useful beam exit port during periods when the beam is not in use.
L.
A suitable irradiation control device must be provided to terminate the irradiation after a preset time interval.
(1)
A timer that has a display must be provided at the treatment control panel. The timer must have a preset time selector and an elapsed time or time remaining indicator.
(2)
The timer must be a cumulative timer that activates with an indication of "BEAM-ON" and retains its reading after irradiation is interrupted or terminated. After irradiation is terminated and before irradiation can be reinitiated, it must be necessary to reset the elapsed time indicator.
(3)
The timer must terminate irradiation when a preselected time has elapsed, if any dose-monitoring system present has not previously terminated irradiation.
(4)
The timer must permit accurate presetting and determination of exposure times as short as one second.
(6)
The timer must not activate until the shutter is opened when irradiation is controlled by a shutter mechanism unless calibration includes a timer error correction to compensate for mechanical lag.
(7)
The timer must be accurate to within 1.0 percent of the selected value or one second, whichever is greater.
M.
The control panel, in addition to the provisions in subpart 2, must have:
(1)
an indication of whether electrical power is available at the control panel and if activation of the x-ray tube is possible;
(6)
for therapeutic radiation machines manufactured after July 9, 1997, a positive display of specific filters in the beam.
N.
When a control panel can energize more than one x-ray tube:
(2)
there must be an indication at the control panel identifying which x-ray tube is activated; and
O.
There must be a means of determining the central axis TSD to within one centimeter and of reproducing this measurement to within two millimeters thereafter.
P.
Unless it is possible to bring the x-ray output to the prescribed exposure parameters within five seconds after the x-ray "ON" switch is energized, the following conditions must be met:
(1)
the beam must be attenuated by shutters having a lead equivalency not less than that of the tube housing assembly;
(2)
after the unit is at operating parameters, the shutters must be controlled by the operator from the control panel; and
Q.
Each therapeutic radiation machine equipped with a beryllium or other low-filtration window must be clearly labeled as such upon the tube housing assembly and must be provided with a permanent warning device on the control panel that is activated when no additional filtration is present to indicate that the dose rate is very high.
Subp. 2.
Facility design requirements.
In addition to shielding requirements of this chapter, the treatment room must meet the following design requirements.
A.
Provisions must be made for continuous two-way communication between the patient and the operator at the control panel.
B.
Provisions must be made to permit continuous observation of the patient during irradiation. The viewing system must be so located that the operator can observe the patient from the control panel. The therapeutic radiation machine must not be used for patient irradiation unless the viewing system is operational.
C.
Treatment rooms, which contain a therapeutic radiation machine capable of operating in a range of 150 kV to 500 kV, must meet the following additional requirements:
(2)
the control panel must be located outside the treatment room or in a totally enclosed booth, which has a ceiling, inside the room;
(3)
interlocks must be provided so that all entrance doors, including doors to any interior booths, must be closed before treatment can be initiated or continued. If the radiation beam is interrupted by any door opening, it must not be possible to restore the machine to operation without closing the door and reinitiating irradiation by manual action at the control panel; and
(4)
when a door is opened while the radiation machine is activated, the air kerma rate at a distance of one meter from the source must be reduced to less than 100 mrad (one mGy) per hour.
Subp. 3.
Full calibration measurements.
A.
Full calibration must be performed by, or under the direct supervision of, a therapeutic radiological physicist:
(1)
before the first medical use following installation or reinstallation of the therapeutic radiation machine;
(3)
before medical use under the following conditions:
(a)
whenever quality control check measurements indicate that the radiation output differs by more than five percent from the value obtained at the last full calibration and the difference cannot be reconciled; and
(b)
following any component replacement, major repair, or modification of components that could significantly affect the characteristics of the radiation beam; and
(4)
notwithstanding the requirements of this subpart:
(a)
full calibration of therapeutic radiation machines with multienergy capabilities is required only for those modes or energies that are not within their acceptable range; and
(b)
if the repair, replacement, or modification does not affect all energies, full calibration must be performed on the affected energy that is in most frequent clinical use at the facility. The remaining energies may be validated with quality control check procedures against the criteria in subpart 4.
B.
The registrant must maintain a record of each calibration for the duration of the registration. The record must include:
(2)
the manufacturer's name, model number, and serial number for both the therapeutic radiation machine and the x-ray tube;
(3)
the model numbers and serial numbers of the instruments used to calibrate the therapeutic radiation machine; and
(4)
the signature or electronic signature of the individual responsible for performing the calibration.
Subp. 4.
Periodic quality control checks.
A.
Periodic quality control checks must be performed on therapeutic radiation machines, subject to subpart 3, which are capable of operation at greater than or equal to 150 kV.
B.
To satisfy the requirements of this part, quality control checks must meet the following requirements:
(1)
the registrant must perform quality control checks according to written procedures established by the therapeutic radiological physicist;
(3)
the acceptable tolerance for each parameter measured in the quality control check, when compared to the value for that parameter determined in the calibration specified in subpart 3, must be stated.
C.
The cause for a parameter exceeding an established tolerance must be investigated and corrected before the system is used for patient or human research subject irradiation.
D.
Whenever a quality control check indicates a significant change in the specified operating characteristics of a system, the system must be recalibrated as required in subpart 3.
E.
The registrant must use the dosimetry system described in part 4732.0925, subpart 2, to make the quality control checks required in this part.
F.
The registrant must have the therapeutic radiological physicist review and sign the results of each radiation output quality control check within one month of test completion.
G.
The registrant must ensure that safety quality control checks of therapeutic radiation machines are performed at intervals not to exceed one month.
H.
Notwithstanding the requirements of this part, the registrant must ensure that no therapeutic radiation machine is used to administer radiation to humans unless the quality control checks required by this part are completed.
I.
Periodic quality control checks must have been performed within the 30 days prior to administration.
J.
Safety quality control checks must ensure proper operation of:
(3)
beam condition indicator lights on the access doors, control console, and in the radiation therapy room;
(5)
if applicable, electrically operated treatment room doors from inside and outside the treatment room.
K.
The registrant must maintain a record of each quality control check for inspection by the commissioner. The record must include:
(2)
the manufacturer's name, model number, and serial number for the therapeutic radiation machine;
(3)
the manufacturer's name, model number, and serial number of the instruments used to measure the radiation output of the therapeutic radiation machine; and
(4)
the signature or electronic signature of the individual who performed the periodic quality control check.
Subp. 5.
Operating procedures.
A.
Therapeutic radiation machines must not be left unattended unless secured by means identified in subpart 1.
B.
When a patient must be held in position for radiation therapy, mechanical supporting or restraining devices must be used.
C.
The tube housing assembly must not be held by an individual during operation unless the assembly is designed to require such holding and the peak tube potential of the system does no exceed 150 kV. In these cases, the holder must wear protective apron and gloves of not less that 0.5 millimeters lead equivalency at 100 kV.
D.
A copy of the current operating and emergency procedures must be maintained at the therapeutic radiation machine control console.
E.
No individual other than the patient must be in the treatment room during exposures from therapeutic radiation machines operating above 150 kV.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.0940 THERAPEUTIC RADIATION MACHINES - PHOTON THERAPY SYSTEMS (500 KV AND ABOVE) AND ELECTRON THERAPY SYSTEMS (500 KEV AND ABOVE).
Subpart 1.
Equipment requirements.
A.
Leakage radiation outside the maximum useful beam in photon and electron modes must meet the following:
(1)
The absorbed dose due to leakage radiation, excluding neutrons, at any point outside the maximum-sized useful beam, but within a circular plane of radius two meters which is perpendicular to and centered on the central axis of the useful beam at the nominal treatment distance, such as patient plane, must not exceed a maximum of 0.2 percent and an average of 0.1 percent of the absorbed dose on the central axis of the beam at the nominal treatment distance. Measurements must be averaged over an area not exceeding 100 square centimeters at a minimum of 16 points uniformly distributed in the plane.
(2)
Except for the area defined in this subpart, the absorbed dose due to leakage radiation (excluding neutrons) at one meter from the electron path between the electron source and the target or electron window must not exceed 0.5 percent of the absorbed dose on the central axis of the beam at the nominal treatment distance. Measurements must be averaged over an area not exceeding 100 square centimeters.
(3)
For each therapeutic radiation machine, the registrant must determine, or obtain from the manufacturer, the leakage radiation existing at the positions in this subpart for the specified operating conditions.
B.
Leakage radiation through beam-limiting devices must meet the following:
(1)
All adjustable or interchangeable beam-limiting devices must attenuate the useful beam such that at the nominal treatment distance, the maximum absorbed dose anywhere in the area shielded by the beam-limiting devices must not exceed two percent of the maximum absorbed dose on the central axis of the useful beam measured in a ten centimeter by ten centimeter radiation field.
(2)
All adjustable or interchangeable electron applicators must attenuate the radiation including, but not limited to, photon radiation generated by electrons incident on the beam-limiting device and electron applicator and other parts of the radiation head, such that the absorbed dose in a plane perpendicular to the central axis of the useful beam at the nominal treatment must not exceed:
(a)
a maximum of two percent of the absorbed dose on the central axis of the useful beam at the nominal treatment distance. This limit must apply beyond a line seven centimeters outside the periphery of the useful beam; and
(b)
a maximum of ten percent of the absorbed dose on the central axis of the useful beam at the nominal treatment distance. This limit must apply beyond a line two centimeters outside the periphery of the useful beam.
C.
Measurement of leakage radiation must meet the following:
(1)
Measurements of leakage radiation through the beam-limiting devices must be made with the beam-limiting devices closed and any residual aperture blocked by at least two-tenths value layers of suitable absorbing material. In the case of overlapping beam-limiting devices, the leakage radiation through each set must be measured independently at the depth of maximum dose. Measurements must be made using a radiation detector with an area not exceeding ten square centimeters.
(2)
Measurements of leakage radiation through the electron applicators must be made with the electron beam directed into the air and using a radiation detector with an area up to, but not exceeding, one square centimeter suitably protected against radiation that has been scattered from material beyond the radiation detector. Measurements must be made using one centimeter of water equivalent buildup material.
D.
Filters and wedges must meet the following:
(1)
Each wedge filter that is removable from the system must be clearly marked with an identification number. For removable wedge filters, the nominal wedge angle must appear on the wedge or wedge tray if permanently mounted to the tray. If the wedge or wedge tray is significantly damaged, the wedge transmission factor must be redetermined.
(2)
If the absorbed dose rate information required by this subpart relates exclusively to operation with a field-flattening or beam-scattering filter in place, the filter must be removable only by the use of tools.
(3)
For equipment manufactured after July 9, 1997, which utilizes a system of wedge filters, interchangeable field-flattening filters, or interchangeable beam-scattering foils:
(a)
irradiation must not be possible until a selection of a filter or a positive selection to use "no filter" has been made at the treatment control panel, either manually or automatically;
(b)
an interlock system must be provided to prevent irradiation if the filter selected is not in the correct position;
(d)
an interlock must be provided to prevent irradiation if any filter or beam-scattering foil selection operation carried out in the treatment room does not agree with the filter or beam-scattering foil selection operation carried out at the treatment control panel.
E.
For equipment manufactured after July 9, 1997, the registrant must determine during acceptance testing, or obtain from the manufacturer, data sufficient to ensure that x-ray stray radiation in the useful electron beam, absorbed dose at the surface during x-ray irradiation, and stray neutron radiation in the useful x-ray beam are in compliance.
F.
All therapeutic radiation machines must be provided with redundant beam monitoring systems. The sensors for these systems must be fixed in the useful beam during treatment to indicate the dose monitor unit rate.
(1)
Equipment manufactured after July 9, 1997, must be provided with at least two independently powered integrating dose meters. Alternatively, common elements may be used if the production of radiation is terminated upon failure of any common element.
(2)
Equipment manufactured on or before July 9, 1997, must be provided with at least one radiation detector. This detector must be incorporated into a useful beam monitoring system. The detector and the system into which that detector is incorporated must meet the following requirements:
(a)
each detector must be removable only with tools and, if movable, must be interlocked to prevent incorrect positioning; and
(b)
each detector must form part of a beam monitoring system from whose readings in dose monitor units the absorbed dose at a reference point can be calculated.
(3)
Each beam-monitoring system must be capable of independently monitoring, interrupting, and terminating irradiation.
(4)
For equipment manufactured after July 9, 1997, the design of the beam-monitoring systems must ensure that the:
(a)
malfunctioning of one system must not affect the correct functioning of the other systems; and
(b)
failure of any element common to both systems that could affect the correct function of both systems must terminate irradiation or prevent the initiation of radiation.
(5)
Each beam-monitoring system must have a legible display at the treatment control panel. For equipment manufactured after July 9, 1997, each display must:
(d)
in the event of a power failure, the beam-monitoring information required in this subpart displayed at the control panel at the time of failure must be retrievable in at least one system for a 20-minute period of time.
(6)
Bent-beam linear accelerators must be provided with auxiliary devices to monitor beam symmetry.
(7)
The devices referenced in this subpart must be able to detect field asymmetry greater than ten percent, and must be configured to terminate irradiation if field asymmetry cannot be maintained at ten percent or less.
G.
Selection and display of dose monitor units.
(1)
The preselected number of dose monitor units must be displayed at the treatment control panel until reset manually.
(2)
After termination of irradiation, it must be necessary to reset the dosimeter display before subsequent treatment can be initiated.
(3)
For equipment manufactured after July 9, 1997, after termination of irradiation, it must be necessary for the operator to reset the preselected dose monitor units before irradiation can be initiated.
H.
For equipment manufactured after July 9, 1997, a system must be provided from whose readings the air kerma rate or absorbed dose rate at a reference point can be calculated. The radiation detectors specified in this subpart may form part of this system. In addition:
(2)
if the equipment can deliver under any conditions an air kerma rate or absorbed dose rate at the nominal treatment distance more than twice the maximum value specified by the manufacturer, a device must be provided that terminates irradiation when the air kerma rate or absorbed dose rate exceeds a value twice the specified maximum. The dose rate at which the irradiation will be terminated must be a record maintained by the registrant;
(3)
if the equipment can deliver under any fault conditions an air kerma rate or absorbed dose rate at the nominal treatment distance more than ten times the maximum value specified by the manufacturer, a device must be provided to prevent the air kerma rate or absorbed dose rate anywhere in the radiation field from exceeding twice the specified maximum value and to terminate irradiation if the excess absorbed dose at the nominal treatment distance exceeds 400 rad (four Gy);
(4)
for each therapeutic radiation machine, the registrant must determine, or obtain from the manufacturer, the maximum values in this subpart for the specified operating conditions; and
(5)
records of these maximum values must be maintained at the facility for inspection by the commissioner.
I.
Termination of irradiation by the beam-monitoring system or systems during stationary beam radiation therapy.
(1)
Each primary system must terminate irradiation when the preselected number of dose monitor units has been detected by the system.
(2)
If the original design of the equipment included a secondary dose-monitoring system, that system must be capable of terminating irradiation when not more than 15 percent or 40 dose monitor units above the preselected number of dose monitor units set at the control panel has been detected by the secondary dose-monitoring system.
(3)
For equipment manufactured after July 9, 1997, an indicator on the control panel must show which monitoring system has terminated irradiation.
J.
It must be possible to terminate irradiation and equipment movement or go from an interruption condition to termination condition at any time from the operator's position at the treatment control panel.
K.
If a therapeutic radiation machine has an interrupt mode, it must be possible to interrupt irradiation and equipment movements at any time from the treatment control panel. Following an interruption it must be possible to restart irradiation by operator action without any reselection of operating conditions. If any change of a preselected value is made during an interruption, irradiation and equipment movements must be automatically terminated.
L.
A suitable irradiation control device must be provided to terminate the irradiation after a preset time interval.
(1)
A timer must be provided that has a display at the treatment control panel. The timer must have a preset time selector and an elapsed time indicator.
(2)
The timer must be a cumulative timer that activates with an indication of "BEAM-ON" and retains its reading after irradiation is interrupted or terminated. After irradiation is terminated and before irradiation can be reinitiated, it must be necessary to reset the elapsed time indicator.
(3)
The timer must terminate irradiation when a preselected time has elapsed if the dose-monitoring systems have not previously terminated irradiation.
M.
Equipment capable of both x-ray therapy and electron therapy must meet the following additional requirements:
(1)
irradiation must not be possible until a selection of radiation type (x-rays or electrons) has been made at the treatment control panel;
(2)
the radiation type selected must be displayed at the treatment control panel before and during irradiation;
(3)
the interlock system must be provided to ensure that the equipment can principally emit only the radiation type that has been selected;
(4)
an interlock system must be provided to prevent irradiation with x-rays, except to obtain a verification image, when electron applicators are fitted;
(5)
an interlock system must be provided to prevent irradiation with electrons when accessories specific for x-ray therapy are fitted; and
(6)
an interlock system must be provided to prevent irradiation if any selected operations carried out in the treatment room do not agree with the selected operations carried out at the treatment control panel.
N.
Equipment capable of generating radiation beams of different energies must meet the following requirements:
(1)
irradiation must not be possible until a selection of energy has been made at the treatment control panel;
(2)
the nominal energy value selected must be displayed at the treatment control panel until reset manually for the next irradiation. After termination of irradiation, it must be necessary to reset the nominal energy value selected before subsequent treatment can be initiated; and
(3)
irradiation must not be possible until the appropriate flattening filter or scattering foil for the selected energy is in its proper location.
O.
Therapeutic radiation machines capable of both stationary beam radiation therapy and moving beam radiation therapy must meet the following requirements:
(1)
irradiation must not be possible until a selection of stationary beam radiation therapy or rotational arc radiation therapy has been made at the treatment control panel;
(3)
an interlock system must be provided to ensure that the equipment can operate only in the mode that has been selected;
(4)
an interlock system must be provided to prevent irradiation if any selected parameter in the treatment room does not agree with the selected parameter at the treatment control panel;
(5)
moving beam radiation therapy must be controlled to obtain the selected relationships between incremental dose monitor units and incremental movement. For equipment manufactured after July 9, 1997:
(a)
an interlock system must be provided to terminate irradiation if the number of dose monitor units delivered in any ten degrees of rotation differs by more than 20 percent from the selected value;
(b)
where angle terminates the irradiation in moving beam radiation therapy, the dose monitor units delivered must differ by less than five percent from the dose monitor unit value selected;
(c)
an interlock must be provided to prevent motion of more than five degrees beyond the selected limits during moving beam radiation therapy;
(d)
an interlock must be provided to require that a selection of direction be made at the treatment control panel in all units that are capable of both clockwise and counterclockwise moving beam radiation therapy; and
(e)
moving beam radiation therapy must be controlled with both primary position sensors and secondary position sensors to obtain the selected relationships between incremental dose monitor units and incremental movement;
Subp. 2.
Facility design requirements for therapeutic radiation machines operating above 500 kV.
In addition to shielding adequate to meet requirements of part 4732.0380, the following design requirements are made.
A.
Protective barriers must be fixed, except for access doors to the treatment room or movable beam interceptors.
B.
In addition to other requirements in this subpart, the control panel must also:
(2)
provide an indication of whether electrical power is available at the control panel and if activation of the radiation is possible;
(4)
include an access control locking device that will prevent unauthorized use of the therapeutic radiation machine.
C.
Provisions must be made for continuous two-way audio communication between the patient and the operator at the control panel. The therapeutic radiation machine must not be used for irradiation of patients unless continuous two-way audio communication is possible.
D.
Windows, mirrors, closed-circuit television, or an equivalent viewing system must be provided to permit continuous observation of the patient following positioning and during irradiation and must be located so that the operator may observe the patient from the treatment control panel. The therapeutic radiation machine must not be used for patient irradiation unless at least one viewing system is operational.
E.
Treatment room entrances must be provided with warning lights in a readily observable position near the outside of all access doors, which will indicate when the useful beam is "ON" and when it is "OFF."
F.
Interlocks must be provided such that all access controls are activated before treatment can be initiated or continued. If the radiation beam is interrupted by any access control, it must not be possible to restore the machine to operation without resetting the access control and reinitiating irradiation by manual action at the control panel.
G.
If the shielding material in any protective barrier requires the presence of a beam interceptor to ensure compliance with part 4732.0380, interlocks must be provided to prevent the production of radiation, unless the beam interceptor is in place, whenever the useful beam is directed at the designated barriers.
H.
At least one emergency power cutoff switch must be located in the radiation therapy room on either side of the primary beam and must terminate all equipment electrical power including radiation and mechanical motion. This switch is in addition to the termination switch required by subpart 1. All emergency power cutoff switches must include a manual reset so that the therapeutic radiation machine cannot be restarted from the unit's control console without resetting the emergency cutoff switch.
I.
Safety interlocks must be designed so that any defect or component failure in the safety interlock system prevents or terminates operation of the therapeutic radiation machine.
J.
Surveys for residual activity must be conducted on all therapeutic radiation machines capable of generating photon and electron energies above ten MV prior to machining, removing, or working on therapeutic radiation machine components that may have become activated due to photoneutron production.
K.
A facility location authorized to use a therapeutic radiation machine according to this part must have at its disposal appropriately calibrated portable monitoring equipment. As a minimum, the equipment must include a portable radiation measurement survey instrument capable of measuring dose rates over the range one mrem (ten µSv) per hour to 1,000 mrem (ten mSv) per hour. The survey instruments must be operable and calibrated at intervals not to exceed 12 months for the radiation measured.
Subp. 3.
Therapeutic radiological physicist support.
A.
The registrant must obtain the support of a therapeutic radiological physicist. The therapeutic radiological physicist must be responsible for:
B.
If the therapeutic radiological physicist is not a full-time employee of the registrant, the operating procedures required by subpart 4 must also specifically address how the therapeutic radiological physicist is to be contacted for problems or emergencies, as well as the specific actions, if any, to be taken until the therapeutic radiological physicist can be contacted.
Subp. 4.
Operating procedures.
A.
No individual, other than the patient, must be in the treatment room during treatment or during any irradiation for testing or calibration purposes.
B.
Therapeutic radiation machines must not be made available for medical use unless the requirements of part 4732.0925 and this part have been met.
C.
Therapeutic radiation machines, when not in operation, must be secured to prevent unauthorized use.
D.
When adjustable beam-limiting devices are used, the position and shape of the radiation field must be indicated by a light field.
E.
If a patient must be held in position during treatment, mechanical supporting or restraining devices must be used.
F.
A copy of the current operating and emergency procedures must be maintained at the therapeutic radiation machine control console.
Subp. 5.
Full calibration measurements.
A.
Full calibration of a therapeutic radiation machine must be performed by, or under the direct supervision of, a therapeutic radiological physicist:
(1)
before the first medical use following installation or reinstallation of the therapeutic radiation machine;
(2)
full calibration must include measurement of all parameters in this chapter. Although it must not be necessary to complete all elements of a full calibration at the same time, all parameters, for all energies, must be completed at intervals not to exceed 12 months, unless the commissioner requires a more frequent interval;
(3)
before medical use under the following conditions:
(a)
whenever quality control check measurements indicate that the radiation output differs by more than five percent from the value obtained at the last full calibration and the difference cannot be reconciled. Therapeutic radiation machines with multienergy or multimode capabilities, or both, must only require measurements for those modes or energies that are not within their acceptable range; and
(b)
following any component replacement, major repair, or modification of components that could significantly affect the characteristics of the radiation beam. If the repair, replacement, or modification does not affect all modes or energies, full calibration must be performed on the effected mode/energy that is in most frequent clinical use at the facility. The remaining energies/modes may be validated with quality control check procedures against the criteria in this subpart.
B.
The registrant must use the dosimetry system described in part 4732.0925, subpart 2, to measure the radiation output for one set of exposure conditions.
C.
The registrant must maintain a record of each calibration for the duration of the registration. The record must include:
(2)
the manufacturer's name, model number, and serial number for the therapeutic radiation machine;
(3)
the model numbers and serial numbers of the instruments used to calibrate the therapeutic radiation machine; and
(4)
the signature or electronic signature of the individual responsible for performing the calibration.
Subp. 6.
Periodic quality control checks.
B.
To satisfy the requirement of this subpart, quality control checks must include determination of central axis radiation output and a representative sampling of periodic quality control checks contained in this chapter. Representative sampling must include all referenced periodic quality control checks at intervals not to exceed 12 months.
C.
The registrant must use a dosimetry system that has been intercompared within the previous 12 months with the dosimetry system described in part 4732.0925, subpart 2, to make the periodic quality control checks required in this subpart.
D.
The registrant must perform periodic quality control checks required by this subpart according to procedures established by the therapeutic radiological physicist.
E.
The registrant must review the results of each periodic radiation output check according to the following procedures:
(1)
the registrant and therapeutic radiological physicist must be immediately notified if any parameter is not within its acceptable tolerance. The therapeutic radiation machine must not be made available for subsequent medical use until the therapeutic radiological physicist has determined that all parameters are within their acceptable tolerances;
(2)
if all quality control check parameters appear to be within their acceptable range, the quality control check must be reviewed and signed by either the registrant or therapeutic radiological physicist within seven working days; and
(3)
the therapeutic radiological physicist must review and sign the results of each radiation output quality control check within 20 working days of completion.
F.
Therapeutic radiation machines subject to this part must have safety quality control checks of each external beam radiation therapy machine performed at intervals not to exceed one week.
G.
To satisfy the requirement of this subpart, safety quality control checks must ensure proper operation of:
(3)
beam condition indicator lights on the access doors, control console, and in the radiation therapy room;
H.
Emergency power cutoff switches must be checked for proper operation at intervals not to exceed three months. If more than one emergency power cutoff switch is installed and not all switches are tested at once, each switch must be tested on a rotating basis. Safety quality control checks of the emergency power cutoff switches may be conducted at the end of the treatment day in order to minimize possible stability problems with the therapeutic radiation machine.
I.
The registrant must promptly repair any system identified in this subpart that is not operating properly.
Subp. 7.
Records.
The registrant must maintain records according to part 4732.0330. The record must include:
B.
the manufacturer's name, model number, and serial number for the therapeutic radiation machine;
C.
the manufacturer's name, model number, and serial number of the instruments used to measure the radiation output of the therapeutic radiation machine; and
D.
the signature or electronic signature of the individual who performed the periodic quality control check.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.1000 REQUIREMENTS FOR X-RAY FLUORESCENT ANALYZERS AND BOMB DETECTION UNITS.
Subpart 1.
Applicability.
This part applies to the use of radiation-producing equipment in x-ray fluorescent analyzers or bomb detection units. The requirements of this part are in addition to any applicable requirements of this chapter.
Subp. 2.
Operating and emergency procedures.
A copy of the registrant's operating and emergency procedures must be available to the employees.
Subp. 3.
Instruction and training.
The registrant must provide initial system-specific training on safe operating and emergency procedures. Additional training must be conducted when any changes in the system occur that would change the quality assurance program. The training must be commensurate with the registered activities. They must include:
A.
procedures for handling and using the radiation-producing equipment so the occupational dose limits in part 4732.0410 are not exceeded;
B.
procedures for controlling the area of use so the limits for the dose to the public in part 4732.0430 are not exceeded;
E.
emergency procedures for the registrant's employees to minimize radiation exposure in the event of an accident or equipment malfunction.
Subp. 4.
Inspection and maintenance of equipment.
The registrant must ensure that:
A.
equipment is inspected prior to initial use and after any changes that would affect the radiation output. The inspection must be done according to the manufacturer's specifications;
C.
the manufacturer or registered service providers are used to conduct repair and maintenance on the system; and
D.
repairs or corrective actions are completed when an inspection reveals a condition that could change the radiation output or increase the dose levels for the occupational worker.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.1040 INDUSTRIAL FACILITY REQUIREMENTS FOR USING RADIATION-PRODUCING EQUIPMENT IN MANUFACTURING PROCESSES, GAUGES, AND CABINETS.
Subpart 1.
Applicability.
This part establishes standards for the use of radiation-producing equipment for manufacturing processes, gauges, and cabinets in industrial settings. The requirements of this part are in addition to other pertinent requirements of this chapter.
A.
A registrant who performs industrial radiography using a certified cabinet system must comply with all requirements of Code of Federal Regulations, title 21, section 1020.40, as subsequently amended.
B.
Individuals who use equipment regulated under this part are not required to hold a radiographer certification.
Subp. 2.
Operating procedures.
The registrant must have operating procedures that include:
A.
maintaining radiation doses as low as reasonably achievable and actions to prevent exceeding the dose limits in parts 4732.0410 to 4732.0430;
C.
identification of the various radiation warning signs, safety devices, and interlocks incorporated into the equipment;
Subp. 3.
Emergency procedures.
The registrant must have emergency procedures that include emergency procedures for employees and the procedures for notifying personnel in the event of an accident or equipment malfunction.
Subp. 4.
Instruction and training.
The registrant must ensure that:
A.
An individual operating or maintaining the radiation-producing equipment is adequately instructed initially in operating and emergency procedures. The training must include:
B.
Additional training must be conducted with the addition of any new radiation-producing equipment.
Subp. 5.
Analytical ionizing radiation-producing equipment.
The registrant must ensure:
A.
any unused ports on radiation-producing housings must be closed to prevent opening by an individual other than the operator;
B.
each port on an open-beam configuration housing must be equipped with a shutter that cannot be operated unless either a collimator or a coupling has been connected to the port; and
C.
the dose does not exceed 0.5 millirem (0.005 mSv) in one hour at a distance of 1.97 inches (five centimeters) from the protective surfaces.
Subp. 6.
Bypassing a safety device.
The registrant must ensure the requirements in part 4732.0630 are met in order to bypass a safety device.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.1050 REQUIREMENTS FOR PERMANENT INDUSTRIAL RADIOGRAPHIC INSTALLATIONS.
Subpart 1.
Applicability.
The requirements of this part are in addition to other applicable requirements of this chapter.
Subp. 2.
Permanent installation; requirement.
All radiographic operations must be conducted in a permanent radiographic installation, unless specifically authorized by the commissioner.
Subp. 3.
Locking of sources of radiation.
The control panel of each radiation-producing machine must be equipped with a locking device that will prevent the unauthorized use of an x-ray system or the accidental production of radiation. The radiation-producing machine must be kept locked and the key removed at all times except when under the direct visual surveillance of a radiographer.
Subp. 4.
Permanent storage precautions.
Radiation-producing machines must be secured while in storage to prevent tampering or removal by unauthorized individuals.
Subp. 5.
Required entrance controls.
An entrance that is used for personnel access to the high radiation area in a permanent industrial radiographic installation must meet the requirements of part 4732.0620, subpart 1.
Subp. 6.
Testing.
A.
The alarm system must be tested for proper operation by energizing the tube each day before the installation is used for radiographic operations. The test must include a check of both the visible and audible signals. Entrance control devices that reduce the radiation level upon entry must be tested monthly.
B.
If an entrance control device or an alarm is operating improperly, it must be immediately labeled as defective and repaired within seven calendar days. The facility may continue to be used during the seven-day period if the registrant implements the continuous surveillance requirements under part 4732.1067.
C.
The registrant must document all instances of interlock or alarm failures, record all corrective actions, and indicate the date that the safety device was restored to working condition.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
October 3, 2013
4732.1055 INDUSTRIAL RADIOGRAPHIC OPERATING AND EMERGENCY PROCEDURES.
Subpart 1.
Operating and emergency procedures.
The registrant must have operating and emergency procedures that include:
A.
operating and safety instructions to maintain radiation doses as low as reasonably achievable and actions to prevent exceeding the dose limits in parts 4732.0410 to 4732.0430;
E.
individual monitoring and the use of individual monitoring equipment, including steps that must be taken by radiography personnel in the event that a pocket dosimeter is found to be off-scale;
Subp. 2.
Radiation surveys and survey records.
The radiation survey requirements in this subpart must be met for industrial radiation-producing equipment.
A.
No radiographic operation must be conducted unless calibrated and operable radiation survey instrumentation, as described in part 4732.0710, is available and used at each site where radiographic exposures are made.
B.
A physical radiation survey must be made after each radiographic exposure using radiation machines to determine that the machine is "off."
Subp. 3.
Calibrated and operable radiation survey instruments.
The registrant must have sufficient calibrated and operable radiation survey instruments accessible at each facility to make a radiation survey as required by subpart 2. Each radiation survey instrument must be calibrated according to part 4732.0710.
Subp. 4.
Utilization logs.
Each registrant must maintain a utilization log for review at the inspection by the commissioner. The log must contain:
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.1058 INDUSTRIAL RADIOGRAPHY IN A TEMPORARY JOB SITE.
Subpart 1.
Applicability.
This part applies to industrial radiation-producing equipment used for less than 30 days at a job site.
Subp. 2.
Restricted areas.
A fence, rope, or other suitable personnel barrier must be used outside the two mR (5.16 x 107 C/kg) in any one hour dose line to restrict entry.
Subp. 3.
Qualified personnel present.
When radiography is performed at a location other than a permanent radiographic installation, the radiographer must be accompanied by at least one other qualified radiographer or a radiographer's assistant. The additional qualified individual must be capable of providing immediate assistance to prevent unauthorized entry.
Subp. 4.
Records for temporary job site.
For records at temporary job sites, each registrant conducting industrial radiography must have available at the temporary job site:
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.1060 INSTRUCTION AND TRAINING FOR INDUSTRIAL RADIOGRAPHY.
Subpart 1.
Registrant requirements.
The registrant must ensure that:
A.
any individual who will be operating or maintaining the radiation-producing equipment is adequately instructed initially in system-specific operating and emergency procedures;
Subp. 2.
Individual requirements.
Ninety days after November 5, 2007, the individual to act as a radiographer must:
C.
be certified through a radiographer certification program by a certifying entity according to part 4732.1070;
E.
demonstrate understanding of the registrant's operating and emergency procedures by successfully completing a written or oral examination covering the material.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.1063 WARNING DEVICES FOR INDUSTRIAL RADIOGRAPHY FACILITIES.
Subpart 1.
Open-beam configurations.
Open-beam configurations must have a readily discernible indication of:
A.
x-ray tube "on-off" status located near the radiation-producing equipment housing, if the primary beam is controlled in an "on-off" manner; or
B.
shutter "open-closed" status located near each port on the radiation-producing equipment housing, if the primary beam is controlled in "open-closed" manner.
Subp. 2.
Warning light.
An easily visible warning light labeled with the words "X-RAY ON" or other visible warning indicator that clearly shows the equipment is producing ionizing radiation, must be located near a switch that energizes an x-ray tube and illuminated only when the tube is energized.
Subp. 3.
Warning device labeling.
Warning devices must be labeled so that their purpose is easily identified.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.1065 POSTING REQUIREMENTS FOR INDUSTRIAL RADIOGRAPHY.
All areas in which industrial radiography is being performed must be conspicuously posted according to part 4732.0385, subpart 4, and this part.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.1067 SURVEILLANCE FOR INDUSTRIAL RADIOGRAPHY.
During a radiographic operation, the radiographer, or the other individual present as required under part 4732.1040, must maintain continuous direct visual surveillance of the operation to protect against unauthorized entry into a high radiation area except at permanent radiographic installations where all entryways are locked and the requirements under part 4732.1050 are met.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.1070 RADIOGRAPHER CERTIFICATION.
Subpart 1.
Requirements for an independent certifying organization.
An independent certifying organization must:
A.
be an organization such as a society or association whose members participate in, or have an interest in, the fields of industrial radiography;
B.
make its membership available to the general public nationwide that is not restricted because of race, color, creed, religion, national origin, sex, disability, sexual orientation, or age;
D.
be an incorporated, nationally recognized organization that is involved in setting national standards of practice within its fields of expertise;
E.
have an adequate staff, a viable system for financing its operations, and a policy and decision-making review board;
F.
have a set of written organizational bylaws and policies that provide adequate assurance of lack of conflict of interest and a system for monitoring and enforcing those bylaws and policies;
G.
have a committee, whose members carry out their responsibilities impartially, to review and approve the certification guidelines and procedures, and to advise the organization's staff in implementing the certification program;
H.
have a committee, whose members can carry out their responsibilities impartially, to review complaints against certified individuals and to determine appropriate sanctions;
I.
have written procedures describing all aspects of its certification program and maintain records of the current status of each individual's certification and the administration of its certification program;
J.
have procedures to ensure that certified individuals are provided due process with respect to the administration of its certification program, including the process of becoming certified and any sanctions imposed against certified individuals;
K.
have procedures for proctoring examinations, including qualifications for proctors. The procedures must ensure that the individuals proctoring each examination are not employed by the same company or corporation, or a wholly owned subsidiary of such company or corporation, as any of the examinees;
L.
exchange information about certified individuals with the commissioner, other independent certifying organization, and allow periodic review of its certification program and related records; and
M.
provide a description to the commissioner of its procedures for choosing examination sites and for providing an appropriate examination environment.
Subp. 2.
Requirements for certification programs.
Certification programs must:
B.
require applicants for certification to provide documentation that demonstrates that the applicant has:
(3)
received verification by the registrant that the applicant has demonstrated the capability of independently working as a radiographer;
D.
include procedures for denying an application and revoking, suspending, and reinstating certifications;
F.
include procedures for renewing certifications and, if the procedures allow renewals without examination, require evidence of recent full-time employment and annual refresher training; and
G.
provide a timely response to inquiries, by telephone or letter, from members of the public about an individual's certification status.
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.1100 INSTALLATION CALIBRATION TESTS AND EQUIPMENT PERFORMANCE TESTS FOR A QUALITY ASSURANCE PROGRAM.
Subpart 1.
Tests required.
A.
Installation calibration tests must be conducted prior to any patient use. Any adjustments must be made to bring the equipment up to a nationally recognized standard such as Code of Federal Regulations, title 21, section 1020, or the manufacturer's specifications, and to ensure compliance with this chapter prior to first use.
B.
Equipment performance tests must be conducted over all clinical ranges, when applicable. For equipment performance tests, any adjustments must be made to bring equipment to a nationally recognized standard or manufacturer's specifications; and to ensure compliance with this chapter prior to using the equipment again.
Subp. 2.
Frequency of tests.
The tests in this part are to be made at the time of installation and at the specified intervals thereafter.
Subp. 3.
Image receptors.
| TEST TYPE | MINIMUM TEST INTERVAL | MINIMUM PERFORMANCE CRITERIA | |
| A. | Screen-film contact | At intervals not to exceed 24 months | No significant areas of poor contact as measured by no less than: (1) 8 wires/inch mesh; or (2) 7 holes/inch for regular film; (3) 40 wires/inch mesh or greater for mammography film |
| B. | Screen-film- cassette speed match |
At intervals not to exceed 24 months | Densities within ± 0.10 O.D. for all cassettes of the same speed used for imaging |
| C. | CR imaging plates | At intervals not to exceed three months or upon observation of image artifacts | Follow manufacturer's recommendations |
Subp. 4.
Processing.
| TEST TYPE | MINIMUM TEST INTERVAL | MINIMUM PERFORMANCE CRITERIA | |
| A. | Darkroom fog | At intervals not to exceed six months | < 0.08 O.D. increase in density (measured at approximately 1.00 O.D.) after 2 minutes using film exposed on-site at the time of test. For mammography the O.D. increase must be < 0.05 |
| B. | Sensitometry and densitometry | Before processing first film of the day | Density difference ± 0.15 O.D. and base + fog + .05 O.D. using film exposed on-site at time of test. Veterinary facilities are not required to perform this test |
| C. | Temperature check | At the time of sensitometry | Follow manufacturer's recommendations |
Subp. 5.
All diagnostic radiographic tubes; required when applicable.
| TEST TYPE | MINIMUM TEST INTERVAL | MINIMUM PERFORMANCE CRITERIA | |
| A. | SID indicator accuracy | At intervals not to exceed 24 months | ± 2% of indicated value |
| B. | X-ray and light field alignment | At intervals not to exceed 24 months | ± 2% of SID any one direction, ± 3% of SID, both directions (total) |
| C. | X-ray and image receptor alignment | At intervals not to exceed 24 months | ± 2% of SID |
| D. | Collimator dial accuracy | At intervals not to exceed 24 months | ± 2% of SID |
| E. | Reproducibility | At intervals not to exceed 24 months | Coefficient of variation < 5% |
| F. | mR/mAs | At intervals not to exceed 24 months | ± 10% of baseline |
| G. | Linearity | At intervals not to exceed 24 months | ± 10% over clinical range |
| H. | Linearity - for mAs only units manufactured after May 3, 1994 | At intervals not to exceed 24 months | Average ratios of exposure to the indicated mAs obtained in any two consecutive mAs settings must not differ by more than 0.10 times their sum, or at two settings differing by no more than a factor of two where the mAs selector provides continuous selection |
| I. | Timer accuracy | At intervals not to exceed 24 months | Single Phase: ± 10% of setting. Three phase, high frequency, and constant potential: use ± 5% of selected time when measured > 100 milliseconds. At times shorter than 100 milliseconds, use manufacturers' specifications |
| J. | Half-value layer | At intervals not to exceed 24 months | Must meet requirements in part 4732.0810 |
| K. | kVp accuracy | At intervals not to exceed 24 months | ± 5% of indicated kVp |
| L. | Phototimer reproducibility, if present | At intervals not to exceed 24 months | ± 5% of average exposure |
| M. | AEC (phototimer) | At intervals not to exceed 24 months | ± 10% of manufacturer's state increments |
| N. | Illuminance of collimator | At intervals not to exceed 24 months | > 15 footcandles |
| O. | Film density vs. thickness change on AEC | At intervals not to exceed 24 months | ± 0.30 O.D. of the averaged exposures over the range specified by the manufacturer |
| P. | Film density vs. kVp change on AEC | At intervals not to exceed 24 months | ± 0.30 O.D. of the averaged exposures when measured at > 1.2 O.D. and over the range as specified by the manufacturer |
| Q. | Spot film reproducibility (fluoroscopy units with manual mode) | At intervals not to exceed 24 months | ± 5% of average exposure |
| R. | Phototimer back-up timer cut off | At time of installation | Terminates exposure at < 600 mAs |
| S. | AEC density at normal or "0" | At intervals not to exceed 24 months | > 1.0 O.D. |
Subp. 6.
For facilities with fluoroscopes and C-arm fluoroscopes, except radiation therapy simulators, manufactured before May 19, 1995.
| TEST TYPE | MINIMUM TEST INTERVAL | MINIMUM PERFORMANCE CRITERIA | |
| A. | Maximum output at tabletop or equivalent minimum SSD | At intervals not to exceed 12 months and every tube change | < 5 R (1.3 mC/kg) per minute for manual; < 10 R (2.6 mC/kg) per minute for automatic exposure rate control systems |
| B. | High level control maximum output at tabletop or equivalent minimum SSD | At intervals not to exceed 12 months and every tube change | < 20 R (5.0 mC/kg-1) per minute |
| C. | Fluoroscopic image size | At intervals not to exceed 12 months and every tube change | Error between fluorographic beam size and observed image size must be no more than ± 3% of SID for all modes and at any tower height |
| D. | Actual spot-film size vs. indicated | At intervals not to exceed 12 months | Error between actual fluorographic beam size at image receptor and indicated image size must be no more than ± 3% of SID for all modes and at any tower height |
| E. | Spot-film reproducibility | At intervals not to exceed 12 months | ± 5% of average exposure |
| F. | Phototimer reproducibility, if present | At intervals not to exceed 12 months | ± 5% of average exposure |
| G. | Fluoroscopic high contrast resolution and distortion | At intervals not to exceed 12 months | Six inch (15 centimeter) intensifier: center 30 and edge 24 (wires per inch) copper mesh; nine inch (23 centimeter) intensifier |
| H. | Half-value layer | At intervals not to exceed 12 months and after every tube change | ± 5% for equipment manufactured before 1973. For equipment manufactured after 1973, follow manufacturer's specified limits |
Subp. 7.
For facilities with fluoroscopes and C-arm fluoroscopes, except radiation therapy simulators, manufactured on or after May 19, 1995.
| TEST TYPE | MINIMUM TEST INTERVAL | MINIMUM PERFORMANCE CRITERIA | |
| A. | Maximum output at tabletop or equivalent minimum SSD | At intervals not to exceed 12 months and at every tube change | > 5 R/min must have automatic exposure rate control; > 10 R/min must have high level control; if not high level control maximum is < 10 R/min |
| B. | High level control maximum output at tabletop or equivalent minimum SSD | At intervals not to exceed 12 months and at every tube change | < 20 R/min |
| C. | All other tests as indicated in subpart 5 | At intervals not to exceed 24 months | See criteria in subpart 5 |
Subp. 8.
For facilities with tomography systems other than computed tomography.
| TEST TYPE | MINIMUM TEST INTERVAL | MINIMUM PERFORMANCE CRITERIA | |
| A. | Section level | At intervals not to exceed 12 months | ± 5 millimeters |
| B. | Level incrementation | At intervals not to exceed 12 months | ± 2 millimeters |
| C. | Section thickness (slice width) | At intervals not to exceed 12 months | Follow manufacturer's specifications |
| D. | All other tests in part 4732.1000 if applicable | At intervals not to exceed 24 months | See criteria in subpart 4 |
| E. | Spatial plane resolution | At intervals not to exceed 12 months | 40 mesh screen or better |
Subp. 9.
For facilities with computed tomography scanners.
| TEST TYPE | MINIMUM TEST INTERVAL | MINIMUM PERFORMANCE CRITERIA | |
| A. | Accuracy of scout localization view | At intervals not to exceed 12 months | ± 1 millimeters |
| B. | Accuracy of distance measurements | At intervals not to exceed 12 months | ± 1 millimeters |
| C. | CT dose index | At intervals not to exceed 12 months | ± 20% from manufacturer's recommendations |
| D. | CT number dependence on slice thickness | At intervals not to exceed 12 months | Mean ± 3 CT numbers averaged over 100 pixels |
| E. | CT number calibration and noise | Daily | Water: 0 ± 5 CT numbers; Noise: ± 3 standard deviations of the mean of the baseline noise variance measurements |
| F. | CT number uniformity and artifacts | Monthly for mobile units. At intervals not to exceed 12 months for fixed base units. | Variation ± 5 CT numbers between the mean values of measurements made at center and edge of phantom that is at least 20 cm. In diameter among a mean of 100 pixels. Artifacts: no noticeable artifacts |
| G. | Hard copy output and visual display | Daily | Luminance and contrast not significantly different |
| H. | Table indexing | At intervals not to exceed six months | ± 0.5 millimeter for each increment |
| I. | Table backlash | At intervals not to exceed six months | ± one millimeter |
Subp. 10.
For facilities with cinefluorographic and special procedure systems.
| TEST TYPE | MINIMUM TEST INTERVAL | MINIMUM PERFORMANCE CRITERIA | |
| A. | Cinefluorographic exposure rates | At intervals not to exceed 12 months | Approximately 10 to 20 µR (2.6 to 5.0 nC/kg) per frame at intensifier for nine inch (23 cm) mode; approximately 20 to 30 µR (5 to 8 nC/kg) per frame at intensifier for six inch (15 cm) mode |
| B. | All tests in subparts 4, 5, and 6, if applicable | At intervals not to exceed 24 months | See criteria in subparts 4, 5, and 6 |
| C. | Film changer screen-film contact | At intervals not to exceed 24 months | No significant areas of poor contact as measured by no less than: (1) 8 wire per inch mesh; or (2) 7 holes per inch |
| D. | High contrast resolution for cinefluorographic and digital systems | At intervals not to exceed 12 months | No significant difference between static and dynamic conditions |
| E. | Optical density of films over duration of filming run | At intervals not to exceed 12 months | < ± 0.2 O.D. difference |
Subp. 11.
For facilities with dental intraoral systems.
| TEST TYPE | MINIMUM TEST INTERVAL | MINIMUM PERFORMANCE CRITERIA | |
| A. | Film processing | Before the first film of the day | Between 0.75 and 1.05 O.D. on the test tool or follow test tool manufacturer's recommendations |
| B. | Fog test | At intervals not to exceed six months | Unable to visualize coin edges |
| C. | Filtration (HVL) | At intervals not to exceed 24 months | Meet requirements in part 4732.0800 |
| D. | Radiation exposure at the end of cone | At intervals not to exceed 24 months | Meet requirements in part 4732.0825 |
| E. | Timer reproducibility | At intervals not to exceed 24 months | ± 10% of indicated timer setting |
| F. | kVp accuracy | At intervals not to exceed 24 months | ± 5% of indicated kVp for equipment manufactured before 1973. For equipment manufactured after 1973, follow manufacturer's specified limits |
| G. | Exposure output reproducibility | At intervals not to exceed 24 months | Coefficient of variation < 5% |
| H. | Dental mA linearity | At intervals not to exceed 24 months | ± 10% over the clinical range |
Subp. 12.
For facilities with dental extraoral systems including panoramic systems.
| TEST TYPE | MINIMUM TEST INTERVAL | MINIMUM PERFORMANCE CRITERIA | |
| A. | Film processing | Before the first film of the day | Use processing as specified in subpart 3. A step wedge may be used. ± one step from standard allowed |
| B. | Fog test | At intervals not to exceed six months | Use criteria in subpart 3, item A, for automatic processing; subpart 4, item A, for manual processing |
| C. | Same test types and minimum performance criteria as in diagnostic radiographic tubes in subpart 4 | At intervals not to exceed 24 months | See criteria in subpart 4 |
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.1120 THERAPEUTIC EQUIPMENT PERFORMANCE TESTS AND LIMITS FOR MEASUREMENT EQUIPMENT.
Subpart 1.
Required tests.
A.
Installation calibration tests must be conducted prior to any patient use. Any adjustments must be made to bring the equipment up to a nationally recognized standard, such as Code of Federal Regulations, title 21, section 892, or manufacturer's specifications and to ensure compliance with this chapter prior to first use.
B.
Equipment performance tests must be conducted over all clinical ranges, when applicable. For equipment performance tests, any adjustments must be made to bring equipment to compliance with a nationally recognized standard, such as Code of Federal Regulations, title 21, section 892, or manufacturer's specifications and to ensure compliance with this chapter prior to using the equipment again.
Subp. 2.
Local standard (Loc. Std.) instrument.
| TEST TYPE | MINIMUM TEST INTERVAL | TOLERANCE |
| A. AAPM - accredited dosimetry calibration laboratory calibration | Intercomparison every 12 months At intervals not to exceed 24 months traceable to NIST Standard |
Documented and correction applied or noted in report of measurement when appropriate |
| B. Linearity | At intervals not to exceed 48 months | 0.5 percent |
| C. Venting | At intervals not to exceed 48 months | Documented and correction applied |
| D. Extracameral signal | Initial use | 0.5 percent |
| E. Leakage | Each use | 0.1 percent |
| F. Recombination | Initial use | Documented and correction applied |
| G. Collecting potential | Each use | Documented and correction applied |
Subp. 3.
Other field instruments.
| TEST TYPE | MINIMUM TEST INTERVAL | TOLERANCE |
| A. Local standard comparison | At intervals not to exceed 24 months | 1 percent |
| B. Linearity | At intervals not to exceed 24 months | Documented and correction applied |
| C. Venting | At intervals not to exceed 24 months | Documented and correction applied |
| D. Extracameral signal | At intervals not to exceed 24 months | Documented and correction applied |
| E. Leakage | Each use | 1 percent |
| F. Recombination | Initial use | Documented and correction applied |
| G. Collecting potential | Each use | Documented and correction applied |
Subp. 4.
Relative dosimetry equipment.
| TEST TYPE | MINIMUM TEST INTERVAL | TOLERANCE |
| A. Thermoluminescent Dosimeter | ||
| (1) Calibration | Each batch or box | Documented and correction applied |
| (2) Linearity | Initial use | Documented and correction applied |
| B. Film | ||
| (1) Dose and response | Each batch or box | Documented and correction applied |
| (2) Densitometer linearity | At intervals not to exceed 12 months | Documented and correction applied |
| C. Air ionization chamber system | ||
| (1) Linearity | At intervals not to exceed 12 months | Documented and correction applied |
| (2) Extracameral signal | Initial use | 1 percent |
| D. Diode system | ||
| (1) Energy dependence | Initial use | Documented and correction applied |
| (2) Extracameral signal | Initial use | Documented and correction applied |
| (3) Linearity | Initial use | Documented and correction applied |
Subp. 5.
Radiation survey instruments.
| TEST TYPE | MINIMUM TEST INTERVAL | TOLERANCE |
| A. Calibration | At intervals not to exceed 12 months | Documented and correction applied |
| B. Linearity | At intervals not to exceed 12 months | Documented and correction applied |
| C. Constancy | Each use | 5 percent |
Subp. 6.
Positioning equipment lasers.
| TEST TYPE | MINIMUM TEST INTERVAL | TOLERANCE |
| A. Accuracy | Daily before patient use | 2 mm |
| B. Hysteresis | Each use | 2 mm |
Subp. 7.
Phantoms and attenuators.
| TEST TYPE | MINIMUM TEST INTERVAL | TOLERANCE |
| A. Thickness | Initial use | Documented and correction applied |
| B. Density | Initial use | Documented and correction applied |
| C. Phantom stacked density | Initial use | Documented and correction applied |
| D. Detector fit | Initial use | Documented and correction applied |
Subp. 8.
Accessory equipment.
| TEST TYPE | MINIMUM TEST INTERVAL | TOLERANCE |
| A. Thermometer calibration | Initial use | 0.1 degree/C |
| B. Barometer (aneroid) | ||
| (1) Calibration Hg | Initial use | 1 mm Hg |
| (2) Intercomparison | At intervals not to exceed 12 months | 1 mm Hg |
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
4732.1130 EQUIPMENT PERFORMANCE TESTS FOR EXTERNAL BEAM TELETHERAPY AND SIMULATION SYSTEMS.
Subpart 1.
Dosimetry.
| TEST TYPE | MINIMUM TEST INTERVAL | TOLERANCE |
| A. Central axis dose calibration | At intervals not to exceed 12 months | 2 percent |
| B. Constancy checks-photons | ||
| (1) Dose per monitor unit along central axis | Weekly | 3 percent |
| (2) Depth dose | Monthly | 2 percent |
| (3) Beam uniformity | Monthly | 3 percent |
| (4) Monitor chamber linearity | At intervals not to exceed 12 months | 1 percent |
| (5) Timer linearity and error | At intervals not to exceed 12 months | 1 percent |
Subp. 2.
Geometry.
| TEST TYPE | MINIMUM TEST INTERVAL | TOLERANCE |
| A. Field positioning aids | ||
| (1) Light field and radiation field agreement | Monthly | 2 mm |
| (2) Mechanical distance pins, lasers, and SSD lights | Monthly | 2 mm |
| (3) Scale readouts | Monthly | 2 mm/1 degree angle |
| B. Machine alignment | ||
| (1) Jaw symmetry | At intervals not to exceed 12 months | 2 mm |
| (2) Coincidence of collimator (jaw) and gantry axes | At intervals not to exceed 12 months | 2 mm |
| (3) Stability of gantry arm and bearing under rotation | At intervals not to exceed 12 months | 2 mm |
| (4) Couch motion and tabletop sag | At intervals not to exceed 12 months | 2 mm |
Subp. 3.
Constancy checks-electrons.
| TEST TYPE | MINIMUM TEST INTERVAL | TOLERANCE |
| A. Beam uniformity | Monthly | 5 percent |
| B. Depth dose | Monthly | 2 mm at therapeutic depth |
| C. Dose per monitor unit constancy check | Weekly | 3 percent |
Subp. 4.
Treatment accessories.*
| TEST TYPE | MINIMUM TEST INTERVAL | TOLERANCE |
| A. Wedge transmission factor | At intervals not to exceed 12 months | 2 percent |
| B. Transmission factor constancy for all treatment accessories | At intervals not to exceed 12 months | 2 percent |
*Attenuation in blocks, wedge factors, and compensator data must be checked annually. A visual inspection of the mechanical integrity of these accessories must be done monthly.
Subp. 5.
Simulators.
| TEST TYPE | FREQUENCY | TOLERANCE |
| A. Localizing lasers | Daily | 2 mm |
| B. Distance indicator | Daily | 2 mm |
| C. Field size indicator | Monthly | 2 mm |
| D. Gantry/collimator angle indicators | Monthly | 1 degree |
| E. Cross-hair centering | Monthly | 2 mm diameter |
| F. Focal spot-axis indicator | Monthly | 2 mm |
| G. Fluoroscopic image quality | Monthly | Established baseline |
| H. Collision avoidance | Monthly | Functional |
| I. Light/radiation field coincidence | Monthly | 2 mm or 1 percent |
| J. Collimator rotation isocenter | At intervals not to exceed 12 months | 2 mm diameter |
| K. Gantry rotation isocenter | At intervals not to exceed 12 months | 2 mm diameter |
| L. Couch rotation isocenter | At intervals not to exceed 12 months | 2 mm diameter |
| M. Coincidence of collimator, gantry, couch axes, and isocenter | At intervals not to exceed 12 months | 2 mm diameter |
| N. Table top sag | At intervals not to exceed 12 months | 2 mm |
| O. Vertical travel of couch | At intervals not to exceed 12 months | 2 mm |
| P. Exposure rate | At intervals not to exceed 12 months | Established baseline |
| Q. Table top exposure with fluoroscopy | At intervals not to exceed 12 months | Established baseline |
| R. kVp and mAs calibration | At intervals not to exceed 12 months | Established baseline |
| S. High and low contrast resolution | At intervals not to exceed 12 months | Established baseline |
Statutory Authority:
MS s 144.12
History:
32 SR 777
Published Electronically:
December 10, 2007
Official Publication of the State of Minnesota
Revisor of Statutes
